There could be no doubt: Lee Gardon had multiple sclerosis.
It was, of course, an agonizing fate to confront, not least because Gardon, 45, had gotten married only months earlier, late in 2005, and seemed finally to have secured a measure of hard-won stability in his life. Gardon was a realist, though, and there seemed to be no use denying the overwhelming evidence. In fact, the diagnosis made such sense, accounted so reasonably for the disparate welter of symptoms with which Gardon had long grappled, that it was likely he had been suffering from MS for some time. He had been an avid athlete since childhood, and remained a gym rat, but as he approached middle age he had come to feel inexplicably “battered and abused” by a variety of pains, sometimes vague, sometimes acute, affecting his joints, his muscles, even his bones. Although he harbored a distrust of traditional medicine, he would periodically relent and seek help from doctors, to little avail. “The doctors I saw weren’t thorough enough,” he complained. “I wanted a complete evaluation, some attempt to put together the pieces of my puzzle, but what I would get was a 30-second visit before the prescription pad came out.” Not infrequently, he would leave the doctor’s office feeling humiliated that his concerns had been diminished.
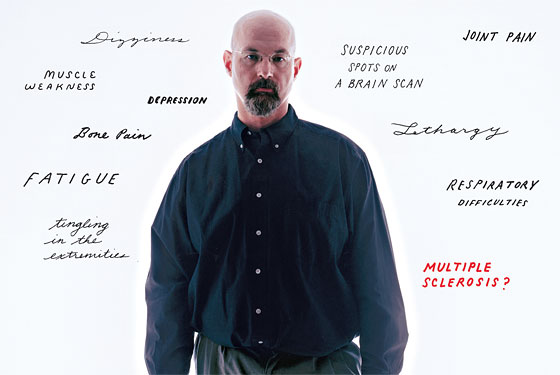
Gardon didn’t look the part of the sickly patient. He stood five feet eleven inches, and seemed fit. He had a vivid, skeptical mind, and spoke in fervent tones about politics, culture, and—his most passionate subject—health. With a shaved head and goatee, Gardon could have been a Lower East Side hipster in an early Jim Jarmusch film. (His Slavic accent was part of the package.) Despite his appearance, though, Gardon was suffering. His symptoms would improve for a while, then suddenly return. By 2005, his pain had become chronic, accompanied by fatigue and lethargy, muscular weakness and respiratory difficulties.
Then, out of the blue, Gardon had a terrible flash of insight into the nature of his problems. He learned that one of his friends, a longtime colleague at the posh New Jersey country club where Gardon works as a purchaser, had been diagnosed with MS. The two men were around the same age. “I was devastated by the news,” Gardon says. In the wake of his sadness for his friend, he came to wonder whether he too had MS. The more he thought about it, the more irresistible the suspicion became. He went online and started researching the disease, and it wasn’t long before he encountered suggestions that it might be caused by exposure to environmental toxins. He was terrified. Before marrying, he had lived for twelve years on the grounds of the country club, in a lodging located near the site where pesticides were stored. He did further research, and learned about cases in which MS was said to have occurred in clusters. “I knew it was highly unlikely that the two of us would develop the disease at the same time,” he reflected, “but it was not out of the question.” He began to monitor his symptoms closely. He had numbness and tingling in his extremities. Sometimes his legs would buckle under him when he attempted to walk. “Man,” he told himself, “it’s highly possible I have this.”
Gardon made plans to see a neurologist. He had a long wait until the appointment, and in the meantime his symptoms grew worse. His wife didn’t know what to think. She accompanied him to the neurologist and implored the physician to put Gardon’s mind at ease by ordering a brain scan. The test produced the outcome Gardon most feared. “The MRI found spots on my brain,” he recounted. In the ambiguous field of MS diagnosis, such lesions, which can indicate the deterioration of the myelin sheath surrounding nerve bundles, are among the strongest findings in favor of the disease. The neurologist, however, cautioned Gardon against seizing on premature conclusions. She told him that the pattern of his lesions was atypical for an MS patient. Nor was she impressed by the coincidence of Gardon’s developing MS at the same time as his friend, or by the array of symptoms he presented. Still, Gardon got his hands on the radiologist’s report, which, as he recalled, concluded, “The possibility of demyelinating disease”—MS—“cannot be excluded.”
“I went to pieces,” Gardon says. He contacted more neurologists, making one, then another, and then another appointment in search of further opinions. The intervals between these appointments stretched on endlessly. Gardon couldn’t imagine living with MS. His late mother, a physiatrist, had treated patients with MS when Gardon was a child, and he retained a memory of these unfortunate people wasting away in wheelchairs. He would go to his office in the middle of the night and spend hours online. Much of what Gardon read seemed merely to confirm the inevitability that he had the condition.
Not surprisingly, Gardon and his wife, Laura, were not enjoying the honeymoon period they might have envisioned. Laura, a massage therapist and aesthetician, had begun to feel that Gardon was drawn to entertaining only the most calamitous scenarios about his health, and her patience with him eroded. She had had plenty of experience with health problems of her own; before meeting Gardon, she had been through two bouts with breast cancer. “I’d had treatments and surgeries,” she says. “I wasn’t happy about any of it at the time, but I dealt with it. It made no sense to me what Lee was going through. To be honest, I got disgusted with it. And then I just became indifferent to him.”
As the months of uncertainty wore on, Gardon withdrew into himself. He was barely functioning. He gave up exercise, took handfuls of tranquilizers to cope with his anxiety, and entered what he called a “zombified” state, unable to turn his mind from thoughts of MS. “I’d be sitting with him,” says Laura, “having a conversation, or watching TV, and suddenly it was as though he wasn’t there at all.”
Laura was beginning to question how long she could remain with Gardon. Then one morning, she picked up a copy of AM New York and spotted an advertisement for a medical-research study that was trying to recruit subjects. She could barely believe what she was seeing.
“Do people call you a hypochondriac?” the ad read.
Not long ago, Lee Gardon would likely have continued to bounce from doctor to doctor, languishing as a lost cause, becoming progressively more isolated and incapacitated by his illness—which, it turned out, was not MS, but rather the extreme, involuntary, unshakable preoccupation with disease that characterizes hypochondria. In this matter, at least, Gardon was lucky. It has long been recognized that hypochondria is neither uncommon nor inconsequential. Chronic worriers represent around 5 percent of patients in primary-care settings, at an estimated annual cost to the health-care system of at least $20 billion in unnecessary doctors’ visits and tests. (One of the few epidemiological studies to address hypochondria, conducted in a community in Vermont nearly 40 years ago, found a 16 percent incidence of hypochondriacal thought.) How to deal with hypochondria, though, has been a far murkier matter. The enduring stigma attached to it has inhibited research and has allowed those who care for (and live with) hypochondriacs to respond to them as though they were toddlers in the midst of tantrums: Ignore them, and after a while, they’ll get over it. Physicians have been known to refer to their hypochondriacal patients as “turkeys,” “crocks,” and gomers (“Get out of my emergency room”), and to pass them on to specialists for further evaluations as a way of getting rid of them. Now, however, after decades of neglect by the medical and psychiatric Establishment, hypochondria is undergoing a paradigm shift. Following the path blazed by such related conditions as depression, anxiety, and obsessive-compulsive disorder, hypochondria is coming to be seen not as a weakness of character or a sign of eccentricity (or, worse, the stuff of a Woody Allen movie) but as a complex phenomenon of neurochemistry, biology, and psychology. The change is anything but academic. It is serving to lend hypochondria a trace of legitimacy, which itself can bring comfort to those who suffer its miseries. And the new model of understanding the causes and processes of rampant illness-related fear has already led to newly effective therapies, and holds out the hope for still more.
Hypochondria has been around, in one conception or another, as long as the practice of medicine. Hippocrates coined the term. Hypo means “under” and khondros refers to the cartilage binding the ribs together; hence, for 2,500 years, the discomfort and malaise of hypochondria was presumed to be situated in the liver, gallbladder, spleen, digestive tract, or other soft abdominal organs from which emotion sprang. Through the nineteenth century, hypochondria was regarded as a sign of intelligence and refinement. James Boswell, who chronicled the minutiae of Samuel Johnson’s thought—including his persistent thoughts of illness—was himself floridly hypochondriacal and particularly concerned with venereal disease. Boswell became the literary muse of medical fretfulness, publishing a series of essays called “The Hypochondriack.” He would keep good literary company: Kant, Darwin, Tolstoy, Charlotte Brontë, Proust, William James, and Tennyson are usually cited on rosters of celebrity hypochondriacs. So is Hitler.
In modern times, hypochondria fell into low esteem and was considered beneath clinical regard; Freud threw up his hands, writing, “I have always felt the obscurity in the question of hypochondria to be a disgraceful gap in our work.” Ironically, its decline seemed to be a function of its comical reputation as a thinking person’s affliction—the furthest thing from an organic illness. Arthur Barsky, professor of psychiatry at Harvard Medical School and director of psychiatric research at Brigham and Women’s Hospital in Boston, admits that it can be a challenge to contest the popular view of hypochondria as a sport of high-strung, hyperbolic, navel-gazing attention-seekers. “Hypochondria is no fun,” he says. “But we’ve still got a long way to go before it’s regarded as a legitimate illness of the brain and not just material for jokes.”
The hypochondriac is a virtuoso of interpretive flourishes, one whose impulse to assign dark meaning to the flotsam and jetsam of bodily sensation is unstoppable. No back pain, stomach discomfort, or patch of dry skin is beneath suspicion, which always inclines toward extravagant causes. Among the most characteristic, and noxious, features of hypochondriacal thinking is its catastrophism. “Hypochondriacs go for diseases that are most dramatic and acute,” notes Brian Fallon, associate professor of clinical psychiatry at Columbia University Medical Center. “They’re drawn to insidious diseases—cancer, MS, heart disease, lupus—that can’t necessarily be identified with 100 percent accuracy by the medical profession, and that affect multiple systems, and have a large variety of symptoms that come and go. In that way, hypochondriacs can always find something to support their fears.” Theirs is a kind of perverse grandiosity, preying on the impossibility of proving a negative. Who can say for sure that one’s body is not being infiltrated by disease? The hypochondriac wades into a spiral of dread, as Barsky says, “because the headache that you think is due to a brain tumor feels a lot worse than the one you think is due to eye strain.” Predictably, hypochondriacs are remarkably vulnerable to bleak suggestion. Hearing about a new threat—SARS, bird flu—can induce panic; glancing at a medical show on television can lead to disease fixation; learning of the illness of a friend or acquaintance can generate a debilitating empathy. (Hypochondriacs often practice elaborate rituals of avoidance—refusing, for instance, to visit sick family members—in an effort to control their fears.) Michael McKee, a Columbia University Medical Center psychologist who has specialized in the treatment of anxiety disorders, points out that there is no safe middle ground for hypochondriacs between perfect health and deadly disease. “The hypochondriac has a thought, and it bursts into flame,” he says.
Just as some people have sharper vision than others, researchers have found that hypochondriacs may be prodigiously attuned to their bodies.
Unwilling to surrender themselves to fate, unable to accept the imperfect authority of medicine, hypochondriacs, Fallon remarks, “suffer from the pathology of doubt and are plagued with uncertainty.” Most can bear their physical symptoms; what they find intolerable is being denied an explanation for what they are feeling. They latch onto a theory about what, for instance, is causing their chest pain—heart failure, anyone?—and then they scan themselves for further signs of the disease. “It’s a disorder of extreme internal vigilance,” says Fallon. “They think they’re facing something that will kill them.” When friends and physicians fail to support their fears, hypochondriacs turn away, feeling resentful and abandoned. They seek comfort, instead, in amateur medical sleuthing. Not long ago, they could be found primarily in the health sections of bookstores and public libraries, furtively poring through reference books. More recently they have taken to wandering the infinitudes of the Internet. “Going online can be a nightmare for the hypochondriac,” Fallon says. “They can spend hours and hours going from site to site. It doesn’t help them feel any better, it often makes them feel worse, and it can totally wreck their home and work life.” Fallon and others call the behavior “cyberchondria.”
Although its features had long been known, it wasn’t until 1980 that the American Psychiatric Association took the first steps to recognizing “hypochondriasis” as a distinct disorder, including it in that year’s edition of the canonical Diagnostic and Statistical Manual of Mental Disorders (DSM) and being careful to distinguish the transient hypochondria that most people experience from time to time—at least 30 percent of patients’ visits to doctors are believed to have no identifiable medical cause—from the hard-core version of the malady. The threshold is high. Not only must the clinical hypochondriac be in the throes of life-altering distress and impairment as a result of an unsupported preoccupation with disease, but the preoccupation has to last at least six months. It takes a lot of stamina to sustain the lonely belief that one is dying for that long. According to Barsky, though, the crucial difference between a casual worrier and a hypochondriac is that the hypochondriac’s imagination of disaster is impervious to rebuttal. “These people are not reassurable,” Barsky says. “For instance: If you notice a mole on your hand, and it seems to have changed, maybe you’ll worry that you have a melanoma. That’s normal. But when you go to get it checked, and your physician tells you it’s not serious, you say, ‘Thank God, that’s what I wanted to hear.’ The hypochondriac responds in the opposite way. Their symptom gets worse.” Indeed, many of the most incorrigible hypochondriacs don’t bother visiting physicians at all. Inconsolable, they keep to themselves, paralyzed by fear that a doctor can do nothing for them but confirm their nightmare.
As the workings of hypochondriacal thought have begun, in recent years, to receive serious attention, much of the research that has emerged takes the form of intriguing hints—suggestions that the brain of the hypochondriac, like that of the person with obsessive-compulsive disorder, becomes an enemy of the restful mind. Barsky and colleagues found that hypochondriacs report higher than average sensitivity to bodily sensations—heat, cold, hunger, noise—and admit to finding minor irritants like insect bites and splinters unusually upsetting. Just as some people have sharper vision than others, Barsky proposes, hypochondriacs may be prodigiously attuned to their bodies. Their problem is that they don’t know how to tune out the bodily “background noise” of daily aches and pains that others barely notice. For the hypochondriac, according to Barsky, “the background static becomes intolerable.” Naturally, what you notice has everything to do with how you feel. James Pennebaker, a psychologist at the University of Virginia, tested two groups of college students on treadmills. One group of the subjects listened to music and street sounds over headphones; another was made to listen to the sounds of their own breathing. There was no difference between the two groups on physiological measures of performance, but those who focused on the sounds of their own bodies reported headaches, racing heart beats, and higher levels of discomfort. The implication, then, is that hypochondria is the product of distorted processes of attention and understanding.
The standard psychoanalytic account of hypochondria maintains that the behavior is an expression of repressed conflicts—unexamined grief, yearning for parental love, distress over real or imagined transgressions. Fallon has seen some patients whose hypochondria can, he believes, be explained in this way. But he has also begun to provide a far more comprehensive account of a range of influences on the development of hypochondria. These include the habit, formed in childhood, of using medical complaints as an effective tool of gaining attention from parents. “These patients don’t even realize that it’s a habit,” Fallon says. “It’s just the way they deal with stress.” Another subgroup of hypochondriacs are strongly akin to obsessive-compulsives, though they limit their fixations to illness. (People with OCD tend to dwell on transmitting a disease, not dying from one.) Yet others have a deeper affinity with depressives. Such hypochondriacs, Fallon says, are often guilt-ridden. “Not uncommonly, it’s someone who has had an affair and is afraid they’ve contracted a sexually transmitted disease. Even though they’ve been to the doctor and are told they’re fine, they can’t stop thinking about it, and it becomes a major source of self-flagellation.” Strangely, some hypochondriacs barely suffer physical complaints at all, but are simply consumed by the thought that something must be wrong with them; across the spectrum, other hypochondriacs focus less on disease than on nagging pains, from which they get no relief, regardless of how many doctors they see or how many tests they are administered. Fallon points to compelling new evidence that the elusive physical ailments with which some hypochondriacs are oppressed might be caused by abnormalities in certain proteins, called cytokines, which are produced by the immune system and help to generate an immune response to disease. Cytokines are believed to cause bodily symptoms like fatigue, pain, and cognitive problems; according to Fallon, it’s likely that a hypochondriac’s brain, beset by abnormal cytokines, could produce such symptoms in the absence of other identifiable causes.
Fallon, whose primary orientation is the overlap between psychiatric and neurological disorders, is working toward providing a description of the neurochemistry of hypochondria that may, ultimately, help to crack the mystery of the disorder. Brain scans, he says, suggest that hypochondria involves a heightening of metabolic activity in the same areas of the brain that are affected in obsessive-compulsive disorder. In OCD patients, this hyperactivity depletes the brain of the neurotransmitter serotonin, which helps to account for the success in treating OCD with serotonin-reuptake inhibitors like Prozac. Fallon was the first scientist to study the effects of such medications on hypochondriacs and has convincingly challenged the traditional notion, supported by cultural and medical prejudice, that hypochondria is untreatable and that its hapless sufferers ought, above all, to buck up. In the late eighties, during his residency at Columbia, Fallon was introduced to a 50-year-old stockbroker with an unwavering belief that he had a brain tumor. The patient had had four brain scans, each of which proved negative, and none of which appeased his fears. He had already received a great deal of psychotherapy and had taken medication for anxiety. Nothing seemed to help. Indeed, given the literature on hypochondria, Fallon himself held out little hope for the man, who was also irritable and unpleasant. As a desperation measure, Fallon’s supervisor, an OCD researcher, suggested administering fluoxetine—Prozac—which was new to the market. In short order, the patient’s worries subsided and his personality was transformed. “Suddenly, he was this gracious, grateful person.”
In 1993, Fallon drew on this success and designed a large-scale study to treat hypochondriacs with Prozac. Within twelve weeks of taking the medication, 70 percent of Fallon’s subjects were substantially relieved of their health-related fears. Given the effectiveness of Prozac for a wide variety of depressive, obsessional, and anxiety disorders, the results were, perhaps, not surprising. Fallon was startled, though, by some of his peripheral findings, which demonstrated the dazzling, and disturbed, powers of the hypochondriacal mind. To begin with, a large number of subjects given a placebo improved just as substantially as those who had been given Prozac. More peculiarly, though, one patient taking the placebo developed an extraordinarily convincing array of the side effects associated with Prozac. Yet another patient, believing she had been switched, midway through the trial, from Prozac to the placebo, underwent a classic case of withdrawal from the drug and suffered a relapse of her hypochondria. It turned out, though, that she had remained on Prozac the whole time.
To complement Fallon’s work, Barsky has demonstrated comparable success in treatments using cognitive-behavioral therapy, which attempts to train patients in techniques to dismantle or circumvent their troubled thought patterns. Brain scans have shown that such therapy has been as effective as Prozac in restoring the hypochondriac’s neurochemistry to normal function. In 2006, Fallon and Barsky decided to pursue the question of treatment further, and joined forces in the largest study ever conducted on hypochondria, a five-year project funded by a grant of more than $5 million from the National Institute of Mental Health. They plan to enroll 264 subjects, and to compare the effectiveness of various therapies and medication separately and in combination. Recruitment of subjects, however, has been slow. Hypochondriacs, being who they are, tend to seek solace in medical, not psychiatric, settings.
Lee Gardon enrolled in Fallon’s leg of the study, conducted under the rubric of the Somatic Disorder and Heightened Illness Concern Research Program at Columbia University Medical Center, in November 2006. By then, Gardon was worried not only about his health but about his marriage as well. He didn’t have much hope for the study, but he had come to a dead end pursuing medical explanations for his illness, and he had to demonstrate to his wife that he was earnestly trying to get better.
Gardon’s skepticism about the study soon began to ease. He was grateful that Fallon’s staff referred to his condition as “heightened illness concern” rather than as hypochondria, a label he found demeaning. During his intake, he responded to a lengthy, detailed survey, and it seemed to him that the kinds of questions it asked—how often he checked himself for symptoms, how focused he was on bodily sensations—reflected an uncanny understanding of his thought process. (Indeed, it turned out that Gardon, who had been a track star in his youth, had been drilled to develop what he called a “hypersensitivity to my body.”) The tone of the questions seemed, Gardon thought, to show some compassion for his ordeals. A psychiatrist administered a physical exam to rule out the possibility of undiagnosed medical conditions. “It was 100 percent different from my other visits to doctors,” he says. “It was very comforting. Apparently, they knew what they were doing.”
Gardon began doing some independent research about hypochondria and was struck by how many risk factors he had for developing the disorder. As many as 70 percent of hypochondriacs are also depressive, and since Gardon’s childhood, in Soviet-dominated Czechoslovakia, he had been described as “melancholic.” Some research has cited a genetic component in hypochondria, and Gardon could recall that his grandfather, with whom he loved to hike in the woods, would carry medication with him on these outings out of fear of having a heart attack. Gardon grew aware, too, that stress could precipitate both physical ailments and a hypochondriacal state of alarm, and his life had featured a litany of hardships: a dramatic and life-threatening escape from Czechoslovakia to Italy, via Hungary and Yugoslavia, in which he ultimately evaded capture by sailing a windsurfer across the Adriatic; two years living in an Italian refugee camp; and the difficulties of arriving alone in the U.S., in 1986, unable to speak English and constantly fearful for his survival. “You have to work long hours and stay healthy if you don’t want to starve,” he says of the experience, “and nobody cares how you feel.”
Indeed, it turned out that the saga of Gardon’s medical woes, which had made him feel so poorly understood, was a casebook study in hypochondria. Constantly fatigued, Gardon had at one point become dependent on stimulants, consuming more than 25 double espressos daily for a long stretch. Anxiety attacks had followed, during which Gardon would be convinced he was having a heart attack. On numerous occasions, he summoned ambulances for himself. Despite tests showing that he had outstanding cardiac health, he worried about his heart so intensely that he installed a GPS unit in his car to map the location of hospitals along his driving routes and avoided crossing bridges and tunnels in case he was stricken while caught in traffic. In time, his health fears had begun to spread. Hearing of an acquaintance’s stroke, he was convinced he was at risk. He feared bone cancer and fibromyalgia. Even the common cold would be a problem—congested, he would grow panicked that his airways were clamping shut.
Gardon was assigned by Fallon’s staff to the group of subjects who would receive both medication and therapy. He was anxious about taking Prozac, given his suspicions of conventional medicine and his concerns about toxins. Still, after years of being regarded as a problem patient, he was now, at Columbia, a model subject, and he complied fully and enthusiastically with the requirements of the study. Each week he headed to the New York State Psychiatric Institute, looming above the Hudson in Morningside Heights, to visit his assigned psychiatrist, with whom he discussed at length his response to the medication. He also had a dozen sessions of cognitive behavioral therapy. In the first session, he was taught deep-breathing techniques that he found effective in short-circuiting panic. He was tutored in common-sense strategies for contending with hypochondriacal thinking, like distracting himself from worry by watching TV or exercising, and placing constraints on his Internet research, and challenging catastrophic thinking with factual information about the likelihood of having a serious disease. Within about a month of starting the study, Gardon felt his hypochondria begin to evaporate. He credited Prozac with the change. After years of believing that he was the victim of a plethora of dire illnesses, Gardon decided, instead, that his principal malady was an easily treated neurochemical imbalance. Gardon had always been in search of a diagnosis, and this one provided him with a powerful explanatory tool for coping with his fluctuating states of mind and body. “It was a revelation,” he says.
It’s not, however, as though Gardon believed he was cured. It will be some years before the results of Fallon and Barsky’s study are published, and for now it remains unclear how long-lasting the effectiveness of either medication or therapy is likely to be. Gardon knows that. And he knows himself well enough to remain ever fearful of the return of crippling anxiety. In March, six months after he wound down his participation in the study, he had surgery to repair a torn rotator cuff. A month later, his arm in a sling, he was paying close attention to how the shoulder was healing. “That’s a habit I can’t break,” he says. His progress was slower than he would have liked, but he claimed not to be unduly worried. Most important, his marriage was much more stable, even if, as Laura, observed, “once the hypochondria improved, there were other issues to deal with, too.” Laura was inclined to attribute Gardon’s hypochondria to the emotional traumas of his past, and those scars had not been made to vanish under the influence of Prozac. Not long ago, Laura says, as the spring allergy season got under way, Gardon woke in the middle of the night in a state of alarm, and repeated a familiar refrain: “I think my throat is closing.”
“I didn’t even stir,” Laura recalls. “In the past, he might have called an ambulance. But this time he just got up and went into the other room. I don’t know what he did out there, but he must have calmed himself down, because the next thing I knew he was back in bed, next to me, sleeping.”