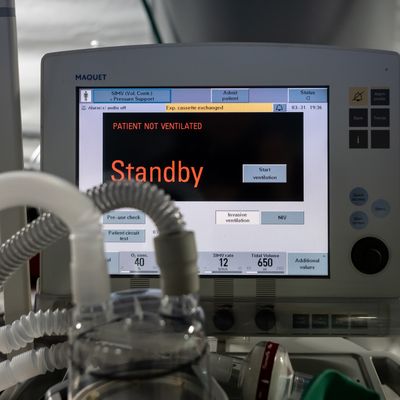
Though the beginning of the week came with some promising signs that the first wave of the coronavirus outbreak may be nearing its peak, the overloading of the American hospital system is far from over. With the apex of the pandemic expected to hit next week, hospitals nationwide may soon face the heart-wrenching decisions made by health-care providers in New York, where one paramedic compared her work last week to “battlefield triage.” Last Thursday, one doctor in New York reported losing a patient due to rationing of ventilators, a choice all too common in northern Italy in March.
While states and the Department of Health and Human Services have provided triage guidelines for natural and man-made disaster scenarios, not all of them have inspired confidence: In Alabama, the plan states that “persons with severe mental retardation, advanced dementia or severe traumatic brain injury may be poor candidates for ventilator support.” To help provide a more ethical framework, The New England Journal of Medicine published guidelines for how to treat patients in hospitals that face ventilator shortages.
In “Fair Allocation of Scarce Medical Resources in the Time of COVID-19,” the authors present a general front for reducing “years of life lost” by prioritizing care for front-line health-care workers who are essential to pandemic response. Behind the workers that keep medical infrastructure intact, resources should then be catered toward “either to the sickest or to younger people who will have lived the shortest lives if they die untreated.” There are some unassailable rules: “Consensus exists that an individual person’s wealth should not determine who lives or dies.” There are also some unexpected recommendations for those outside the medical community, as the authors suggest that a first-come, first-served mentality — which governs most nonemergency situations — actually introduces more bias into the system.
To help understand the recommendations, Intelligencer spoke with bioethicist and oncologist Ezekiel Emanuel, the leading author on the New England Journal of Medicine paper. Emanuel — a universal-health-care advocate who helped write the Affordable Care Act, working in the Obama administration with his younger brother Rahm — explained some of the decisions that doctors across the country may soon face.
Are there substantial differences between previous triage guidelines that you’ve written and the current outbreak, or is the only profound change the lack of resources?
That’s a big difference, but even in a moderate flu pandemic, we would have had some major supply issues. But the point is that we as doctors have not generally had a situation where we’ve had real resource scarcity. We do have it in transplantation, but, you know, you see these minor — I don’t want to trivialize them — but you see cases all the time. The ICU is full and you’re admitting patients. What do you do? How do you manage that? Those are real cases, people work around the edges, they figure out how to make do. But they are a kind of triage.
What’s interesting is that in the medical profession, outside of our papers, there hasn’t been that much written on this. There has been a series of reports, but we haven’t educated doctors about this. We haven’t done those kind of things, and now we need to, quite clearly we need to.
Why isn’t it built into the education?
The need hasn’t been present. I did teach a course precisely on this issue, called rationing and resource allocation, to get doctors and nurses and other people to really think through what these choices that we have to make are and how to make them. But I think it’s not part and parcel of regular medical school. I still think that’s mostly because we thought we were so rich, we thought the system was so well resourced we wouldn’t have to make those choices, and doctors really didn’t. Even though if you talk to the transplant people, they’re doing it all the time.
In the past, you’ve written critically about tying health care to employment in the U.S. Do you feel that this situation would be alleviated in some capacity if there were universal care?
No doubt. That’s like open and shut. I don’t think there’s any question about that. But is it making it worse? This is a worldwide phenomenon. We’re having it worse because we haven’t had leadership. Would it have been complicated even with different political leadership? For sure. With H1N1 in 2010, it was still hard even with a competent president engaged. There’s always other stuff presidents are worried about, attuned to. What is interesting is that H1N1 never pushed everything else out of the news; they were still working on ACA, the bailout from the recession. But this has pushed everything else off the front page.
The article states that “consensus exists that an individual person’s wealth should not determine who lives or dies.” How would you describe, then, what happened to a 17-year-old in Lancaster, California, who died six hours after he was turned away from a private hospital because he did not have insurance?
Look, that it shouldn’t happen and that it does are two different things. I think there is universal agreement that your ability to live or die should not be dependent on your financial well-being. Financial well-being tends to be highly a matter of inheritance and luck, and those are not relevant criteria for living or dying.
Could you explain why, for patients with similar prognoses, random allocation is better than first come, first served, which seems like the given process in so much of life?
Because first come, first served is a terrible allocation system. It’s just that simple. It’s [a system] that maybe is okay in theory, but we have at least three reasons to think in practice it’s wrong. First of all, it biases toward people that are near facilities. Second, it biases the sort of people who may have been irresponsible and got infected first, versus the people who were doing the physical distancing and did everything right then by chance got it. I was just hearing from someone in Israel, while the Orthodox have somewhat ignored the physical-distancing requirements, so they’re getting sick a lot, so they’re first come. But that’s exactly rewarding the wrong behavior, and it tends to do that all the time. The last is that we know that in practice, first come, first served almost invariably prioritizes well-off people. They know how to manipulate the system, how to get their way to the front of the line, that’s how they walk the race of life. So you’re just compounding that bias.
Could you speak to the potential of the psychological trauma for clinicians as they have to make these decisions?
Look, every physician I know lives with a decision or a set of decisions he or she made that just gnaws at them. Did they do the right thing? Did someone suffer unnecessarily or maybe even died because of either them or someone close to them made a decision? They feel the worst possible that someone might die because of a decision they have to make. And it’s a decision where they don’t control all the variables, they’re being forced to make a decision because of the shortage of ventilators, people, whatever it is. That will haunt people for the rest of their lives — there’s just no doubt about it. I’ve talked to psychiatrists and they think this is like PTSD for doctors and nurses waiting to happen.
This interview has been edited for length and clarity.