On August 3, 2012, the Food and Drug Administration approved a new cancer drug called Zaltrap as a safe and effective treatment for patients with advanced colon cancer. The approval was based on a large-scale clinical trial that showed that Zaltrap, given in combination with three previously approved drugs to patients who had failed initial therapy, extended median overall survival by 42 days.
No one knew the price of Zaltrap at that point, but Leonard Saltz, who heads the gastrointestinal oncology group at Memorial Sloan-Kettering Cancer Center, had a sense of what was coming. Zaltrap’s effectiveness, in his opinion, was almost identical to that of Avastin, an FDA-approved cancer drug that had also been targeted at that same patient population. Several weeks earlier, Saltz had traveled to Chicago to inflict a little premonitory sticker shock on his medical colleagues. He reviewed the recent clinical results of both Zaltrap and Avastin when used as a “second line” treatment, after initial treatment had failed. As Saltz reminded the other oncologists, Avastin was modestly effective as a second-line treatment—it extended median overall survival by 42 days, the same as Zaltrap—but it cost about $5,000 a month and, like Zaltrap, would have to be taken for many months to achieve that modest clinical benefit. The overall cost was so high that Saltz devoted the end of his talk to a back-of-the-envelope calculation, delivered via PowerPoint, that recast the question in terms of health-care costs: If you extended the 42 days survival to a year, “what is the cost of Avastin for one year of human life saved?”
The answer was astounding, even to doctors who have grown inured to the zero-gravity economics of cancer pharmaceuticals. As Saltz worked his way through slide 73 of 78, he arrived at the bottom line: $303,000.
“Now, that’s essentially the cost of the bare-bones drug,” Saltz later explained to me in his office at Sloan-Kettering. “It’s parts, not labor. No money for doctors; no money for nurses; no money for pharmacists; no money for real estate, heat, and lights; no money for the needles, the IV tubing, the IV fluids, the anti-nausea medicines, the other chemotherapies that are given, because Avastin doesn’t do anything by itself. It has to be given with other drugs … I want to emphasize it’s not that we can have a year of life saved for $303,000. That’s probably less than half of what the actual cost would be when you factor in everything.” Zaltrap, he figured, was probably going to be in the same range.
Saltz’s message was not entirely unexpected. He has been warning about the danger of rising drug prices, to patients and to the health-care system in general, for the last decade. Having made this point to his colleagues, Saltz packed up his computer, took the next flight back to New York, and, after the FDA approved Zaltrap in early August, began to prepare—“not with great enthusiasm,” he conceded—the Zaltrap presentation he would deliver to the hospital committee responsible for approving any new drugs for Sloan-Kettering’s pharmacy.
Then, on August 31, he received an e-mail from a pharmacist at the hospital about the price that Zaltrap’s manufacturers, Sanofi and Regeneron Pharmaceuticals, had set. The pharmacist said, in effect, “Are you aware that this drug is twice as expensive as Avastin?”
“No,” Saltz replied, “I wasn’t aware.”
The pharmacist e-mailed the numbers, and Saltz stared at the figures on his computer screen. Zaltrap, the drug that was extremely similar to Avastin, cost roughly $11,000 a month. (And because that extra 42 days wouldn’t be possible without taking the drug for, say, seven months before—which was roughly what was happening in clinical trials—the price for that six-week life extension could be as high as $75,000.)
“Wow,” he said to himself, “that’s a deal-changer for me.”
That may not seem like a heretical statement, but the unspoken rule in American health care is that doctors should never consider the cost of a medicine that might be beneficial to patients. When the FDA approves a new cancer drug, it analyzes safety and effectiveness only. Medicare is obliged to reimburse payment for the drug, and private insurers in most states must cover the cost. Any doctor who considers cost—or the value of a costly drug—risks being accused of “rationing” health care.
Saltz felt compelled to consider the cost. He didn’t see any medical advantage to Zaltrap for his patients—or any disadvantage, for that matter—but, as he contemplated its price, he thought, I can’t see why I would use this.
That same day, he sent an e-mail to every physician at the hospital who treated patients with colon cancer. “I said, essentially, ‘You all know the data. You were at the meetings. You know what the situation is. What I just learned is this issue regarding the price. Within this context, I can’t envision a scenario where I would plan to use this drug. Can you?’ ”
None of the sixteen colon-cancer physicians at Sloan-Kettering who replied to Saltz’s query said they could see a reason for using the drug.
The hospital’s Pharmacy and Therapeutics Committee met in September 2012 to decide whether to include Zaltrap in their list of medications, and Saltz, who chairs the committee, informed his colleagues of the price and recommended not carrying the drug. The committee agreed. Sloan-Kettering, one of the country’s preeminent cancer hospitals, would not be offering Zaltrap to its patients.
When Saltz called upstairs to inform Peter B. Bach, director of the Center for Health Policy and Outcomes at Sloan-Kettering, of the decision, Bach wanted to know the reason.
“Because of the price,” Saltz told him.
As soon as he heard that, Bach, who has been documenting the dizzying rise of cancer-drug prices since 2009, immediately jumped into an elevator to go to Saltz’s office to learn more about the unprecedented decision. Why the rush? “C’mon!” Bach explained to me recently. “It’s never happened before! Sloan-Kettering isn’t including a drug because of its price?”
Thus began the first physician-initiated revolt in anyone’s memory against the skyrocketing cost of cancer drugs.
“Everybody agrees: The prices are unsustainable,” Saltz said. “And I often try to invite myself or people having these discussions to complete the thought: If it’s unsustainable, what happens when it’s unsustained? Do we have an adjusted, steady correction? Or do we have an implosion and a crash?”
Every time there is a public debate about drug prices, the pharmaceutical industry replies, as it did to the Zaltrap episode, with several fundamental arguments: The cost of bringing a new drug to market is enormous—$1.3 billion per drug, according to one often-cited (but often-contested) academic study; the drugs provide value and address unmet patient needs; and, perhaps most important, high prices—and profits—are necessary to subsidize the innovation that allows the industry to bring newer, better medicines to market. After Sloan-Kettering’s decision, Sanofi also pointed out in a statement that Zaltrap demonstrated “important survival benefits” for patients with metastatic colon cancer and provided an important treatment option (a company spokesperson declined to answer any further questions about the pricing of Zaltrap for this story). Usually, after these arguments are made, the debate dies down and prices continue to go up.
Cancer drugs have become a very big business, even though they serve what one expert has described as a “boutique” market. An estimated 1.7 million Americans will be diagnosed with cancer this year, according to the National Cancer Institute, and more than 580,000 people will die from some form of malignancy. In 2012, the overall market for “oncologics” reached nearly $26 billion a year in the U.S. alone, and annual global sales are projected to total $85 billion by 2016, according to the IMS Institute for Health Informatics.
What is sobering about this booming business is that, as a group of oncologists wrote earlier this year, “most anti-cancer drugs provide minor survival benefits, if at all.” They often (but not always) reduce the size of inoperable tumors, but they rarely eradicate the disease. For relatively uncommon malignancies like testicular cancer, some forms of leukemia, and lymphoma, drugs effectively cure the disease; for the common “solid tumor” cancers (lung, breast, colon, prostate, and so on), which account for the vast majority of annual cases, drugs buy some time—precious time, to be sure, but time usually measured in weeks and months rather than years. And even though many of the newer drugs are less toxic, they often still have to be given with older drugs whose side effects include nausea, hair loss, fatigue, and decreasing blood counts. One anti-cancer drug produces a skin rash so severe and disturbing, according to Saltz, that some patients have been asked by employers not to come to work.
In 1965, at the dawn of Medicare, the chemotherapy drug Vinblastine cost $78 a month, according to a widely cited Sloan-Kettering price compendium. In 2011, Bristol-Myers Squibb introduced a new melanoma drug called Yervoy at a cost of about $38,000 a month for a three-month treatment.* Yervoy followed, by about a year, a new prostate-cancer therapy called Provenge that cost $93,000 per course of treatment. Even an ancient chemotherapy like nitrogen mustards, cousins to World War I’s mustard gas and in use since 1949, have gotten caught in the cost updraft; in 2006, a course of treatment experienced a thirteenfold price increase, from $33 a month to $420 a month.
And it’s not just that the price of cancer drugs has doubled in the last decade—it’s that the rise in prices, according to cancer doctors, has far exceeded the drugs’ effectiveness. In 1994, the median survival rate for someone with advanced colon cancer was eleven months, according to Saltz, and the lifetime costs of the drugs used to treat the average patient would be about $500 at today’s prices. By 2004, the median survival rate had increased twofold, to 22 months, but Saltz says the drug costs had increased hundreds of times for that extra eleven months.
*This article has been clarified to show that the $38,000 per-month cost for Yervoy is for a three-month course of treatment.
Richard Larson, an oncologist at the University of Chicago Hospital, says the Zaltrap episode was “a shot across the bow” of the health-care community, “making people start to think that there needs to be some sort of limit on costs,” especially for drugs with “such a marginal benefit.” But the problem, according to Saltz, is much bigger than one drug. “Zaltrap is simply a little piece of the puzzle,” he says. “The prices of cancer drugs in general, I believe, are inappropriately high.”
Explaining how cancer-drug prices have become “inappropriately high” is complicated, and there is more than one explanation. To a colon-cancer expert like Saltz, it is the story of drugs that cost too much and do too little. To a leukemia expert like Hagop Kantarjian, of MD Anderson Cancer Center in Houston, it is conversely the story of drugs that are spectacularly effective but cost so much that they threaten to bankrupt the patients whose lives they have miraculously prolonged. To a health-care-policy analyst like Peter Bach, it is the story of a market so jerry-rigged with regulations that, as a graduate-school professor once told him, “the beautiful thing about health care is that it has every market failure you’ve ever heard of—plus two or three more.”
To an oncologist like Deborah Schrag, of the Dana-Farber Cancer Institute in Boston, who first warned nine years ago in a New England Journal of Medicine editorial that increases in prices of colon-cancer drugs were far outstripping increases in clinical benefit, it is the story of a kind of reimbursement shell game, where most patients are buffered from the high cost of drugs (and health care in general) by third-party payers. As the Affordable Care Act begins its fitful rollout, some health-care experts are expressing concern about a crazy quilt of plans on health-insurance exchanges where patients enrolled in some state plans may pay modest amounts for drugs (New York plans call for a $70 co-pay on cancer drugs), while patients in other states might pay considerably higher rates.
And because the economics of cancer drugs have always been colored by emotion, where patients facing a grim prognosis are desperate to try anything (as are their doctors), it is also a story of misunderstanding what many of these drugs can and can’t do. Last year, Schrag published a stunning study in the New England Journal of Medicine reporting that 81 percent of patients with advanced colon cancer (and 69 percent of patients with advanced lung cancer) did not understand that the drugs used in their treatment would not cure them. “People really anchor on cancer as a disease that causes so much suffering that patients are willing to bankrupt themselves to try something,” says Rena Conti, a health-care economist at the University of Chicago. “There is an irrationality about it, which is quite natural but feeds into this willingness to pay for anything.”
For those reasons and others, the average price of cancer drugs has gone “through the roof,” according to George W. Sledge Jr., former president of the American Society of Clinical Oncology. “What predicts the price of the next cancer drug is the price of the last cancer drug,” says Bach. “The only check on the system is corporate chutzpah.”
In 1957, a chemotherapy drug named 5-fluorouracil was patented, and by the sixties “5-FU,” as the drug is commonly called, had quickly become the first choice of oncologists in treating colon cancers and related gastrointestinal malignancies. It usually didn’t cure the disease once the cancer had spread; it temporarily blunted the disease’s progression. Over the ensuing decades, massive amounts of 5-FU have been used to treat colon cancer, which strikes about 145,000 Americans each year.
The same year 5-FU was patented, Saltz was born in New York. He grew up in Westchester County, went to Horace Mann, attended Stanford, got his medical degree at Yale, began to specialize in oncology, and since 1989, has treated colon-cancer patients at Memorial Sloan-Kettering. And 5-FU, Saltz admits, is “a drug that’s very embarrassing to people like me.”
Now 56 years old, just like Saltz, the drug continues to be “the best and most important drug we have to treat colorectal cancer,” he says. “Every drug that has come along since was designed to replace it and failed and wound up finding a niche by adding to it.” The newer medications—including Avastin and Zaltrap—have become part of combination therapies, but, as Saltz says, drug cocktail has come to mean “a combination of drugs that don’t work well enough to do the job by themselves.”
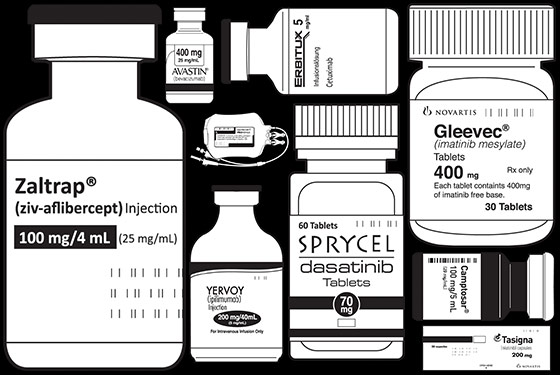
That didn’t stop pharmaceutical companies from charging top dollar for new colon-cancer drugs that did not live up to expectations. The FDA approved Camptosar in 1996; until it went generic, the Pfizer drug cost about $5,300 a month, and it extends median overall survival by, at best, 90 days, according to Saltz. Avastin was approved in 2004; the Genentech drug now costs about $5,000 a month (based on Sloan-Kettering’s analysis), and it extends average survival by, at best, 141 days as a first-line treatment and by about 42 days as a second-line treatment. ImClone, a biotech company, won approval for Erbitux in 2004; Bristol-Myers Squibb and Eli Lilly, which acquired ImClone, now market the drug for about $8,400 a month; the best-case study, according to Saltz, extends median survival by 120 days. Some follow-up studies, he adds, show less of an overall survival benefit. Moreover, virtually none of the newer drugs extends survival without being used with other chemotherapy, usually 5-FU, which currently costs about $30 per treatment. The IV apparatus, Saltz says, is probably more expensive than the drug.
Saltz acknowledges that cancer research is incredibly difficult and that progress is neither easy nor cheap, but he once believed that the drugs developed over the last twenty years, based on elegant new molecular biology, would revolutionize treatment and make the use of 5-FU and other chemotherapies seem like an archaic practice by medical Druids. “These were going to make us look back and say, ‘Can you believe we used to give drugs to people that made their blood counts drop and made them vomit and made their hair fall out? Now we block the blood supply to the tumor! We turn off the growth-factor receptor! It’s so much better! It’s so much less toxic! It’s so much more effective!’ ” Saltz says. “That’s what we all envisioned. That’s not what happened.”
The only part of the vision that came true was that the drugs were so much more expensive. “When these drugs failed—and they did fail—to replace the drugs before them,” Saltz says, “the fallback position was: Let’s see if the [old] drugs plus the new drug are better than the [old] drugs alone. And that’s how these drugs come to market … We start out with a new drug and get excited about it. We do big expensive studies with high hopes for it. And the drug winds up doing less than we hoped it would, but it gets on the market, and then it is both hyped and billed as if it did what we hoped it would do in the first place.” (Pharmaceutical companies, not surprisingly, disagree with Saltz. “A person diagnosed with advanced colorectal cancer can now be expected to live for two years, and each of these medicines have contributed to that,” says Charlotte Arnold, a spokesperson for Genentech, which manufactures Avastin. “I think that when we talk about what we gain as a society, we should be looking at the big picture. As a society, our investment in new drugs and new medicines has been paying off.”)
In the battle against terminal illness, of course, a patient’s calculus of cost effectiveness often has more to do with living to see a child’s graduation or a spouse’s birthday than with the median survival benefit, and reaching those milestones is worth every penny. But as Saltz and other doctors are increasingly pointing out, the cost is steep both to society (in terms of those third-party pennies) and to patients (in terms of quality of life). “You might live 60 days longer,” says Bruce Hillner of Virginia Commonwealth University, “but the evidence suggests that each of those 60 days was diminished in some meaningful way” by the side effects of the drugs. Just last week, a New England Journal of Medicine editorial characterized high drug prices as a form of “financial toxicity.”
Saltz takes these failures a little personally, because he played a major role in bringing some of these medicines to market. He led key clinical trials resulting in FDA approval for two of them (Camptosar and Erbitux) and has conducted clinical trials with Avastin, too. And, like many oncologists, he keenly feels the emotional cost of resorting to treatments he wishes were more effective. Hence, these words—mind you, from the chairman of the Pharmacy and Therapeutics Committee at a hospital that likes to think of itself as the premier cancer center in the world: “Whereas we had hoped that small, incremental gains would be a springboard to something bigger and more productive, I fear those small, incremental gains have become a business model. Right now, it is safer for a pharmaceutical company to strategize for large-scale clinical trials that look for small, incremental gains that will get a drug to market, than to swing for the fences and try for the big advance.”
It’s not just that the skewed market for cancer drugs rewards mediocre products, he says. “Mediocrity is so well rewarded that it’s a better risk than aiming higher.”
A lot of what determines the price of cancer drugs can be attributed to the byzantine economics of health care: markets that don’t behave the way “real world” markets do; artificial price supports that are called something else; government regulations that remove any downward pressures on pricing; and, until Medicare reforms kicked in, in 2005, arcane reimbursement policies that actually rewarded oncologists who used higher-priced drugs, because it would increase the profit margins of their practices. You practically have to become a health-care economist to understand how it works, which is exactly how Bach, who trained as a pulmonary physician, became Sloan-Kettering’s in-house expert on cancer-drug pricing.
In 2009, Bach published an article on cancer-drug prices in the New England Journal of Medicine that documented their dramatic rise and tried to explain the reason for it. The article laid out the tangled, almost Rube Goldberg regulatory strictures that shape—or, more accurately, distort—the cancer-drug market. The foundation for that market is the patent system, which rewards innovation by granting monopoly status to a new drug and essentially allows drug companies to name their price during the period of market exclusivity, generally seven to twelve years. It continues with federal limitations on Medicare that prevent the government’s largest purchaser of cancer drugs from negotiating with drug-makers on price.
The centerpiece of the 2009 article was a chart tracking the price of every cancer drug approved by the FDA since 1965 (now regularly updated by Bach and his colleague Geoffrey Schnorr). In preparing it, Bach discovered several dirty secrets about drug pricing. The first is that there is no fixed price. The “sticker price” of a cancer drug is listed in a compendium called the Red Book, but no one pays that price, according to experts. Drug companies can, and do, offer undisclosed discounts to health-insurance companies, hospitals, and middlemen in the health-care market. So prices vary widely. The Sloan-Kettering compendium pegs its cancer-drug prices to Medicare reimbursements, which give an indication of the real marketplace price (and the cost to taxpayers). These prices are lower than those in the Red Book, but still, according to Bach, are “astronomical.”
Second, the chart documents a recent sea change in pricing. It shows a very slight uptick in prices until the mid-eighties, when the rise becomes more substantial, and then bends sharply upward around 2000. Beginning about twenty years ago, the graph also shows a series of dots way above the curve of average prices, indicating drugs that, in effect, have broken the sound barrier on price since the nineties.
“Then one day I looked at the whole landscape,” Bach recalled, “and thought, Huh, I now know why cancer-drug prices are so high. Because the entire regulatory environment is structured in a way where there are no downward pressures and there are no standards. Medicare—and most private insurers, who want to do business in most states—have to include every drug in coverage. And they have to pay the producer’s price. It’s kind of that simple.”
Bach, incidentally, doesn’t fault the pharmaceutical companies for continuing to push the envelope on pricing. They have a responsibility to shareholders to maximize their profits, he says, and “are responding in a logical way” to an illogical system that, in terms of prices, has “no upper limits. They’re just going to creep up as fast as they can get away with.”
He also realized that one of the few downward-market pressures on pharmaceutical prices was what he calls “headline risk”—an economist’s way of saying “negative publicity.” And that’s why he raced down to the tenth floor when Saltz called him about the Zaltrap decision. It was an opportunity to make some public noise in the drug-price debate.
Saltz proposed writing a joint commentary about Sloan-Kettering’s Zaltrap decision for the Journal of Clinical Oncology, where cancer doctors have been venting about high prices for years. (In a 2009 JCO editorial, Hillner and his colleague Thomas J. Smith criticized the rise in cancer-drug prices with this statement: “Profiteering, the act of making a profit by methods considered unethical, such as raising prices after a natural disaster, is a pejorative term that we believe can be applied to this recent trend where a life-threatening disease is the natural disaster.”)
Despite this rising discontent in the medical literature, Bach knew that no one besides doctors would read a medical journal, so he argued instead for approaching the Times with the idea of announcing Sloan-Kettering’s Zaltrap decision as an op-ed piece signed by Saltz, Bach, and Robert Wittes, then physician-in-chief of the hospital. In the piece, which appeared last October, they wrote, “When choosing treatments for a patient, we have to consider the financial strains they may cause alongside the benefits they might deliver.”
Several weeks later, citing “market resistance,” Sanofi cut the price by 50 percent—an unprecedented discount for a cancer drug. Sloan-Kettering still does not carry Zaltrap.
When Hagop Kantarjian, who heads the Department of Leukemia at the University of Texas’s MD Anderson, saw the op-ed, and the effect it had on the drug’s price, he was both surprised and heartened. “Before that,” he says, “all the previous efforts by doctors had been halfhearted and not successful.” As several health-care economists pointed out in the wake of the Zaltrap episode, hospitals could use their pharmacies as a way to hold the line on drug prices, and physicians could take the lead in highlighting the problem. So Kantarjian said to himself, “What if you took one disease, and all of the experts in the field advocated against high drug prices? If they could do it, why not us?” Us was an international group of experts on leukemia. But these doctors picked an entirely different fight with the pharmaceutical industry: They wanted to highlight the problem of high prices for really effective drugs.
Over the past decade, Kantarjian watched in disbelief as the cost of a successful leukemia drug called Gleevec rose. “I was shocked that it had tripled since 2001,” he says, “and there was no reason for the increase in price, except that the companies could do it and nobody could do anything about it.” Kantarjian, as established a figure as there is in American oncology, suddenly became radicalized.
He drafted a letter protesting the high prices of certain leukemia drugs and began showing it to colleagues, including Richard T. Silver of New York Presbyterian–Weill Cornell Medical Center. The issue clearly touched a nerve with other doctors. “At first the group was kind of small,” Silver says, “and then everybody wanted to be on the bandwagon.” By the time the letter appeared last April in Blood, the field’s primary journal, Kantarjian had collected 119 signatories on six continents, including doctors at Massachusetts General Hospital, the Mayo Clinic, and the Fred Hutchinson Cancer Research Center in Seattle.
The doctors confined their argument to drugs for chronic myelogenous leukemia (CML), a cancer of the blood that strikes roughly 5,000 Americans each year. But they suggested that the pricing of CML drugs bordered on profiteering, because patients now have to take these very expensive drugs continuously, for years, if they want to stay alive. When Gleevec, the first successful CML drug, came out in 2001, the annual sticker price was $30,000, they noted; by 2012, it had risen to $92,000 a year. Moreover, Kantarjian said, three new second-generation CML drugs, approved in 2012, all have list prices around $100,000 a year. (The Sloan-Kettering analysts price these drugs at less than the Blood editorialists, although Bach agrees that the prices for CML drugs are exceptionally high.) “The financial picture is completely different from ten years ago,” Kantarjian says.
Unlike the drugs with “modest” colon-cancer benefits, Gleevec is arguably the biggest success story in cancer therapy in the last fifteen years. Practically overnight, it changed chronic myelogenous leukemia from a devastatingly fatal disease in which less than 20 percent of patients were still alive ten years after diagnosis to essentially a chronic illness in which more than 80 percent of those diagnosed are alive ten years later. “A hugely successful drug,” says Ellin Berman, a CML expert at Sloan-Kettering. “Really a home run.”
So why would more than 100 international leukemia experts, including Berman, sign the Blood editorial and take the pharmaceutical industry to task about such a marvelous class of drugs? One reason, of course, was the sheer financial burden of having to take a $100,000-a-year drug for the rest of one’s suddenly extended life. But the biography of Gleevec also undermines two key arguments used by the drug industry to justify high prices: that those revenues justifiably reward innovation and that the free market ultimately establishes a fair price.
The compound now known as Gleevec was originally designed by chemists at the Swiss company Ciba-Geigy (which later merged with another company to form Novartis). But Ciba-Geigy balked at developing the drug because it considered the CML market too small, even though enterprising research by physician Brian Druker, first at Harvard and then at the Oregon Health & Science University, showed the drug to be remarkably effective against human leukemia cells. “To me, this was the innovation, and this was the risk,” Druker told me recently, “and I was dealing with one of the most risk-averse companies in the world.” For nearly five years, Druker relentlessly pressured Ciba-Geigy, and then Novartis, to allow him to test the drug in human patients. For five years, the companies refused.
Finally, in 1998, after Druker essentially challenged Novartis to test the drug or license it to a company that would, the company relented, fully expecting the drug to fail, according to Druker and others. But even the early Phase I results, usually limited to establishing safe dosages, produced spectacular results: Higher doses of the drug sent 53 of 54 patients with a previously incurable form of cancer into remission. Last year alone, Gleevec racked up sales of about $4.7 billion for Novartis, and the success of the drug opened the door to the development of five second-generation CML drugs—all with a sticker price around $100,000.
This early history is one of the reasons Druker is so frustrated by the current pricing situation and why he, too, signed the Blood editorial. “I would have thought more drugs would have meant more competition, and that more competition would have meant prices coming down. But here, prices keep going up.” If you want to see how a free market operates for Gleevec-like drugs, Kantarjian suggests looking at South Korea. That’s because a South Korean drug company independently patented and developed a second-generation CML drug and priced it at about $21,500 a year, according to Kantarjian. As a result, all the competing CML drugs are priced between $21,000 and $28,000—a quarter of what the same drugs cost for American cancer patients.
And these high prices in the U.S. may now be having negative consequences, both financial and medical. Patients with cancer are 2.5 times as likely to declare bankruptcy as the general population, according to a recent study led by Scott Ramsey of the Fred Hutchinson Cancer Research Center. Monthly co-pays for an $8,000-a-month drug can be financially onerous, especially for people known as “naked patients”—those who aren’t wealthy enough to have supplemental health insurance and not poor enough to qualify for Medicaid. Kantarjian said a disturbing new trend has emerged; some middle-class patients saddled with these continuing co-payments—up to 10 percent of CML patients, by his estimation—are beginning to discontinue a lifesaving treatment because of the out-of-pocket cost, after which the cancer develops resistance to the drug and they can no longer be treated.
In response to the Blood editorial, Novartis issued a statement saying that sustainability of the health-care system is a “complex topic” and that the company’s “critical role … is to discover and develop innovative treatments.” Novartis also noted its “patient access programs,” which help patients cover the high cost of their medications. Many pharmaceutical companies have such patient-assistance programs. Economists like Bach consider these programs a form of artificial price supports that allow the companies to keep overall prices high.
It was precisely these financial issues that led to a little literary tiff between Kantarjian and Silver over the wording of the Blood editorial. Kantarjian insisted that the high prices of CML drugs were forcing doctors to violate the Hippocratic oath (“First, do no harm”). Silver disagreed.
“I thought using the Hippocratic oath was inappropriate,” Silver says, so he told Kantarjian: “Hippocrates meant ‘Do no harm’ from a medical point of view.” Kantarjian replied, “If you kill a patient financially, that counts too.”
Kantarjian has brought a rhetoric to the price debate that is unusual for such a prominent figure in oncology. He accuses the pharmaceutical industry of “greed” in its pricing of CML drugs, argues that “there is zero correlation—zero—between how effective a drug is and the cost of the drug,” and becomes especially indignant when pharmaceutical-industry spokespeople suggest that any effort to contain drug prices will curtail innovation, calling it a form of “blackmailing” against the national interest. He’s pretty exasperated with his fellow oncologists, too. “In the last decade, we have become glorified employees of the drug companies,” he says.
Since the Blood editorial, Kantarjian has begun to talk to other disgruntled physicians, including a doctor concerned about the price of a new drug for a blood disorder called paroxysmal nocturnal hemoglobinuria (which costs a staggering $523,000 a year) and a pair of cystic-fibrosis physicians who published an editorial in the Journal of the American Medical Association on October 2 lamenting the $311,000-a-year cost of a “personalized medicine” drug for the disorder. Kantarjian, meanwhile, is trying to spread his “cut the price” gospel. He’s going to be speaking to a group of health-care executives at the end of October in Chicago and wants to enlist oncologists who specialize in the skin cancer melanoma. Yervoy now costs about $39,000 a month, and a promising new class of drugs called PD-1 inhibitors, currently in advanced testing, is expected to cost even more. (“I mean, why not?” Bach says. “No one is going to stop them.”) “We’ve come to an intolerable situation,” says Kantarjian.
Fueled by his concern for both patients and the health-care system, he is helping to organize a meeting in Washington, D.C., in December of what he calls “stakeholders” in the drug-price debate—doctors, patients, health insurers, federal regulators, and, of course, the drug companies—to “begin the dialogue” about high drug prices; the Leukemia & Lymphoma Society is planning a similar initiative. Kantarjian favors the creation of a governmental “value-based system” to set drug prices on the basis of medical benefit. “New drugs should be evaluated by a committee of experts,” he says, “who can say, ‘This is how much it improves survival, and this is how much the price should be.’ ”
Such a committee already exists in England. Its technical name is the National Institute for Health and Clinical Excellence, or NICE, and it considers not only the benefit but also the cost in deciding what drugs will be covered by the U.K.’s National Health Service. Its decisions allow an implicit form of government negotiating over the price of drugs, because when NICE has turned down a drug as having too little clinical bang for the buck, companies have often come back to the panel with a lower price.
As a result, a British cancer patient usually pays substantially less than American patients. Gleevec costs about $33,500 a year in England, according to NICE; the U.S. price ranges up to $92,000 (according to the Blood editorial). Tasigna, a newer CML drug, costs about $51,000 in England, while the U.S. price ranges up to $115,000. Sprycel, another new CML drug, costs nearly $49,000 a year in England, while the U.S. price ranges up to $123,000.
More to the point, NICE has recently said no where Medicare has been forced to say yes. In January 2012, NICE declined to approve Avastin for both colon and breast cancer, and last June, NICE reached the same conclusion about Zaltrap as Sloan-Kettering’s physicians—it declined to cover the use of the drug, considering it too expensive.
“One of my many politically incorrect opinions,” Saltz says, “is that NICE is an undesirable but necessary inevitability.” The notion that something like NICE could be imported to this country is anathema to the pharmaceutical industry and a pipe dream to most American health-care economists, but Saltz believes we need to start talking about the price tag.
“There is a number in people’s minds,” he says. “If you say to people, ‘I have a drug that extends life by one day at a billion dollars; shouldn’t we as a society pay for it?,’ I’m pretty confident most people would say no. If I say, ‘I have a drug that extends life by three years at a cost of $1.50,’ I’m pretty confident everybody would say, ‘Of course!’ Somewhere in there is a number, a tipping point, where we say, ‘No, we can’t.’ Right now, we’re unwilling as a society to explore where that point is. And I would argue that we have to. Wherever it may be, we have to find it.”
Two Cancer Drugs:
A Brief History
Zaltrap:
Prescribed for: Metastatic colon cancer
Year it came to market: 2012
Original sticker price: $11,000 per month
Current market price: $6,500 per month (after company discounted the price)
Median survival benefit: 42 days
Gleevec:
Prescribed for: Chronic myelogenous leukemia
Year it came to market: 2001
Original sticker price: $30,000 per year
Current market price: $92,000 per year
Current price in the U.K.: $33,500 per year
Median survival benefit: Puts the disease into indefinite remission