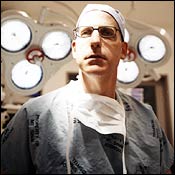
INNOVATOR: ANEURYSMSLucille Ball died of an abdominal aortic aneurysm. So did George C. Scott and Albert Einstein. “It would be interesting to speculate how Einstein’s mind would have benefited mankind for another few years,” says Michael Marin, the founder of Mount Sinai Hospital’s program in endovascular surgery and a pioneer in repairing abdominal aortic aneurysms.
When arteries weaken, one of the most common trouble spots is a section of the aorta, the main pathway from the heart to the legs, just below the kidneys. An abdominal aortic aneurysm forms when the affected portion of the artery balloons out, leaving the artery vulnerable to rupture. More than 200,000 abdominal aortic aneurysms are diagnosed annually. If detected in advance (with a CT scan or a sonogram), the condition is treatable in 95 percent of the cases. Undetected aneurysms, however, can rupture, and ruptures kill 75 percent of the people who experience them.
Most abdominal aortic aneurysms occur in older men, like the patient Marin came across as an attending surgeon at Montefiore Medical Center in 1992. He was too ill for conventional surgery, so Marin began looking for alternatives. After a few months of searching, Marin found an Argentine surgeon named Juan Parodi, who had invented a new, minimally invasive technique, which Marin brought to Montefiore.
Marin inserts a stent- graft—a sort of artificial artery made of polyester fitted over a stent—into the abdominal aorta via two small incisions in the patient’s groin. The graft is positioned at the site of the aneurysm, where it pops into place and serves as a sort of artery within an artery—the aneurysm is bypassed, and blood flows through the graft instead. Surgery that used to involve a two-week hospital stay and several months’ recovery time now has patients out of the hospital the next day, and recovery takes less than two weeks. For older patients with other medical problems, the risk of postoperative mortality has been reduced from nearly 15 percent to less than 2 percent.
A tinkerer by inclination, Marin spent years building and refining his own stent-grafts by hand. Now a device he’s importing from Israel may hold even more promise. Marin has recently become the first doctor to implant an intravascular telemetric monitor, which warns of leakage in patients with aortic stent- grafts. The device, which looks—and to some extent works—like a microchip, lies dormant on the graft’s surface until an ultrasound machine signals it to take pressure measurements on the old aneurysm, which are then transmitted back to doctors (if the stent-graft is working properly, there should be no undue pressure on the damaged part of the artery). Unwieldy and expensive follow-up CT scans to check that the stent-graft is working may soon be unnecessary. That means “cost reduction, safety, and, most important, convenience to the patient,” says Marin.
Eventually, Marin hopes, the telemetric monitor can be calibrated to measure, and possibly even respond to, glucose levels, pH levels, and other key indicators of health. “Think about it,” he says. “There’ll be a time when we no longer have to give blood tests in order to analyze body chemistries. We’ll press a small ultrasound device on your belly and it will tell us everything.”
