
(Photo credit: Eugene Richards)
On an evening in mid-November 2001, Gil Lederman made a judgment call that would bring him the kind of fame that even he had never dreamed possible. A bespectacled cancer doctor with an Alfred Kinsey fade haircut, Lederman was already something of a local celebrity; his distinctive nasal monotone had been heard for years on New York talk-radio stations, promoting his revolutionary cancer treatment, fractionated stereotactic radiosurgery, at Staten Island University Hospital. But Lederman’s fame—as a kind of Dr. Zizmor of radiation oncology—paled in comparison with that of his patient, George Harrison, who was lying in a rented house near the hospital, dying of lung cancer that had invaded his brain.
Though he’d been treating Harrison for only about a month, Lederman thought they had bonded enough to warrant an unconventional house call. “I feel like a brother to him,” the doctor confided to another physician at his hospital. So, as any man with an ailing sibling would do, Lederman showed up that night on Harrison’s doorstep with his three children in tow, so that they might say hello and good-bye to Uncle George, who was leaving the next morning for California, where he would die two weeks later.
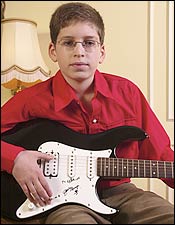
That night has become something of an outer-borough Rashomon. Depending on whose version you believe, Lederman either had a touching visit with Harrison or bullied a dying man in a declining mental state into creating a valuable piece of rock-and-roll memorabilia. The Harrison camp claimed as follows: Lederman showed up uninvited and instructed his 13-year-old son, Ariel, to strum a song on his Yamaha electric guitar. When the performance was over, Lederman put the guitar in Harrison’s lap and asked him to sign it. “I do not even know if I know how to spell my name anymore,” responded an exhausted Harrison. “C’mon, you can do this,” said Lederman, guiding his hand and spelling his name aloud: G-E-O-R-G-E H-A-R-R-I-S-O-N.
Lederman insisted to friends that Harrison invited the children over and happily signed the guitar. The shaky scrawl of the signature itself is inconclusive—it could have been written under duress or simply signed by a willing star on a great deal of medication. Nevertheless, once the Harrison estate sued the doctor for $10 million and the press got their mitts on the legal complaint, Lederman became a popular tabloid target. At the peak of the frenzy, he was labeled a “ghoul” and a “scumbag.” “Page Six” even ran a cartoon depicting him chasing Keith Richards with a pen and guitar. “I’m not on my deathbed!” Richards yells.
It seemed like the ultimate disgrace for a Harvard-trained, triple board-certified physician who should have been amassing yacht money or doing Lasker Award–quality research at that point in his life. Then again, Lederman’s behavior at Harrison’s deathbed wasn’t a complete surprise to those who’d been watching his curious approach to his career. “My sense of the guy is that he’s just somebody who doesn’t get it,” says a prominent radiation oncologist who’s met him on several occasions. “His social skills aren’t there.” But it turns out that questionable manners may be the least pernicious of Lederman’s sins. The doctor is now facing half a dozen multi-million-dollar civil suits, some of which accuse him of bilking terminal cancer patients by luring them with promises of a miracle cure.
As Dr. Lederman waxed on about his mother, George Harrison, according to a source, spoke three measuredwords: “Please…stop…talking.”
Lederman’s defenders claim that the Harrison matter has turned a caring, innovative physician into the kind of wounded game that trial lawyers love to hunt. “Lederman prides himself on taking the most challenging cases that nobody else wants, cases where patients have not been given any hope whatsoever. He’s not offering them a cure but an option,” says Andrew Garson, an attorney who defended Lederman in two previous malpractice cases and believes the recent spate of lawsuits stems from his client’s bad press. Even a judge weighing a recent change-of-venue request acknowledged that Lederman had been through the ringer. His decision played off Harrison’s “Something”: “Something in the folks he treats / Attracts bad press like no other doctor.”
But others contend that the Harrison case was just a symptom of Lederman’s larger pathology of being singularly unable to grasp right and wrong when dealing with the fragile emotions of desperately ill people. “The real issue with Gil is the following,” says Jay Loeffler, chief of radiation oncology at Massachusetts General Hospital. “Is he a genius, far ahead of his time? Or is he a scoundrel?”
Lederman grew up a bookish Jew surrounded by the flinty Protestants of Waterloo, Iowa. His Ukrainian-immigrant grandfather had started a small clothing concern called Lederman’s Western Outfitters, where young Gil earned a nickel an hour. (This explains the geeky scientist’s incongruous fondness for Western shirts and ornate cowboy boots.) He decided he wanted to be a doctor when he was 12 years old. It was 1966, the year the Beatles released Revolver, and his older brother was nearly killed by a drunk driver. “At that moment I decided that I wanted to help people,” he says.
He trained in three specialties—internal medicine at the University of Chicago–Michael Reese Hospital, then medical oncology and radiation oncology at Harvard—and at the age of 34 became the director of Staten Island University Hospital’s radiation oncology department. Though it’s rare for a doctor who’s never practiced full-time to be the director of a program, it wasn’t exactly a prestige post. Before Lederman’s arrival in 1987, the radiation oncology department was just what you’d find in most community hospitals; that is, if you lived on Staten Island and your kid needed radiation, you’d wait about five seconds before driving to Sloan-Kettering or New York-Presbyterian. The department had a single aging cobalt machine and saw only eleven patients a day.
The ambitious new director set out to change that. Lederman forged a close relationship with then–hospital CEO Rick Varone, and, over the next decade, persuaded the administration to buy five linear accelerators, at $1.8 million a pop. In 1991, Lederman became the first doctor in New York to offer brain radiosurgery. Unlike standard radiation treatment, which irradiates a large field around a cancer, exposing healthy tissue to low doses of toxic radiation, radiosurgery is designed to zero in on the tumor. Finely shaped radiation beams are sent into the head from many different directions, with the full dose concentrated where they intersect. The upshot is that larger doses can be trained on the cancer, while healthy tissue is minimally affected. Lederman describes it with an elegantly simple metaphor: “Imagine a plum in a bread box … Radiosurgery can hit the plum without attacking the bread box.”
Still, the machines were worth nothing unless they had bodies to aim at, so Lederman started spreading the gospel of radiosurgery, for which he charged about $18,000 per round of treatment. “My feeling was, if you have a new treatment, then people should learn about it,” he says. “We were educating people.” There were radio ads, cable-television spots, Internet advertising, and presentations at the hospital. Lederman also went on tour, traveling to Italy, England, Israel, and many other countries to speak to prospective patients and examine their CT scans on the spot.
As time went on, these talks were organized by “Lederman clubs,” groups of grateful former patients who would show up to provide testimonials. “I believe in the nineteenth century they called that a medicine show,” says Jonathan Behrins, a Staten Island trial lawyer suing Lederman on behalf of nine Italian patients. “It’s got all the trappings of a classic con.”
Like any businessman, Lederman knew that testimonials work even better when they come from celebrities. He turned the walls of his waiting room into the kind of celebrity shrine you see in Italian red-sauce joints. Sick and dying patients could behold signed photos from the hodgepodge of luminaries he’d treated or met: Curtis Sliwa praised his “brainiac doc” near photos of Lederman chatting with Rudy Giuliani, not far from the shot of Marilyn Quayle visiting the department. Henry Kissinger, Elie Wiesel, and Charo received equal places of honor.
Lederman’s canny sense of self-promotion seemed to be paying off. By the late nineties, as many as 140 patients would cycle through the department on a given day. The linear accelerators whirred and pivoted around their bodies from 6 A.M. to midnight, five nights a week, and even on Saturdays. The hospital started an International Patient Program and opened an office in Naples, Italy. Soon, sick people from all over the world were flying in. Even an ailing Beatle was willing to give the magic ray gun a shot. Lederman was summoned to the Harrisons’ Swiss villa to make his case for treatment.
Once Harrison arrived in Staten Island, Lederman basked in his reflected limelight. He told a friend that he was spending so much time with the rock star that his kids wondered if he’d ever be home to cook dinner again. “Gil said George Harrison didn’t want anybody else taking care of him,” the friend says. “He wanted Gil to be on 24/7.” When Harrison needed to pee, Lederman was there with a plastic urinal. Lederman told another doctor that Harrison offered to autograph things for him, saying, “I can make you a very rich man,” and that Lederman had politely declined: “I’m already a rich man. I don’t need you to autograph for that purpose.”
Some doctors who saw the two together say they looked like close friends. “That’s ridiculous,” says another source who was at the hospital every day. “You might have seen Lederman behaving tenderly. But George was barely coherent at times.” Lederman, the source says, spent only about three hours total in Harrison’s presence, and his behavior was “cloying.” As for that close bond? The morning before Harrison left the hospital, Lederman came into his room in a bright mood. As the doctor waxed on about his mother, Harrison, according to the source, spoke three measured words: “Please … stop … talking.”
But it wasn’t these interactions that set off alarm bells in the Harrison camp; it was the feeling that Lederman intended to use Harrison to promote his treatment. Before long, Lederman popped up on The Early Show with Bryant Gumbel, who introduced him as the doctor treating Harrison. And when the rock star died, Lederman gave touching anecdotes to Good Morning America, CNN, NBC, Fox News, Us Weekly, Newsweek, the New York Post, the Daily News, a variety of British tabloids, and the National Enquirer, which somehow got the erroneous impression that Harrison had been convalescing in Lederman’s own Staten Island home. He told reporters about the spiritual quest that led Harrison to India, how the Harrison he knew was a simple man who would have been happy planting trees, and how Harrison was in no pain and wasn’t afraid of death. He even allowed the Enquirer into his home to take a photo of his son, Ariel, playing the guitar that generous George had signed for him. Of course, many of the stories also mentioned Lederman as a “top cancer specialist” who “pioneered” a “revolutionary cancer surgery” that had a “90 percent success rate.”
“Look,” says Dr. Lederman, “just becausesomeone died doesn’t mean they died of thecancer or the treatment.”
The exceedingly private Harrison family, however, wasn’t interested in allowing the former Beatle to become Lederman’s pitchman from the great beyond. To stop the doctor from talking about her dead husband, Olivia Harrison filed a complaint with the State Board of Professional Medical Conduct, which fined and censured Lederman for revealing too much about his patient. To prevent the autographed guitar from potentially ending up on eBay, she slapped him with a $10 million lawsuit. (As part of the settlement, Lederman relinquished the guitar and agreed not to speak further about Harrison or the case.) The same week the case was filed, SIUH announced that Lederman would be replaced as director of radiation oncology.
According to a doctor at the hospital, Lederman blamed this unfortunate series of events on the fact that Olivia Harrison was “a little jealous that [George’s] attention was being devoted more to Gil than to her.”
To put it kindly, Lederman seems to have a creative relationship with the facts, whether about his friendship with a former Beatle or the possibilities of a cancer treatment. From the beginning, the way that Lederman and the hospital advertised radiosurgery raised eyebrows in the medical community. “I’d pick up the Sunday Times and see these bold advertisements that said, ‘If you’ve been told you have an incurable brain tumor, come to Staten Island University Hospital,’ ” says Loeffler. “I thought that was a little deceptive, because if you’ve been told this, the reality is that it’s probably true.”
But true to his advertising, and for whatever it’s worth, Lederman was willing to treat patients whom most doctors would turn away. “How do you say to a patient, ‘Go home and die; we’re not willing to try’?” asks Bruce Tannenbaum, SIUH’s former manager of radiation oncology. “It’s not doing any harm, so it’s not unethical to do.” But another former colleague took a dimmer view of the program’s acceptance policy: “I got the impression that if a stray dog had insurance, Lederman would treat it.”
Depending on your point of view, when it comes to new technologies, Lederman is either a forward-thinking early adopter or unacceptably reckless. In 1996, he learned that at Sweden’s Karolinska Institute, where radiosurgery had been invented decades before, two doctors had published preliminary results of a trial in which they used the same treatment on tumors below the neck. It was a controversial procedure because the body could not be stabilized as well as the brain: Organs move around, as much as a centimeter even in a restful state; the brain stays put. But the Swedes had received FDA approval for a device that they claimed stabilized the body enough to make radiosurgery both safe and effective. While many doctors weren’t yet convinced, Lederman, who had been performing brain radiosurgery for years, believed it would work on the body as well. He called Varone from Sweden to tell him about the revolutionary new treatment. Within two months, before there had been any independent scientific studies, Lederman became the first doctor in the United States to offer body radiosurgery.
And of course, he wasted no time in marketing the hell out of it. Any patient who called a toll-free number received a glossy pamphlet and video touting the procedure’s successes, followed by a personal call from the doctor himself. With liver metastases, which typically indicate an aggressive cancer, “we have a success rate of 95 percent,” says the pamphlet, which defines “success” as any cancer that shrinks, or at least remains the same size. How about pancreatic cancer, perhaps the most quick and deadly of them all? “Over 94 percent of primary pancreas cancers have been successfully controlled in the treated area.”

If the data weren’t convincing enough, the infomercial-style video would hammer the point home. In it, Lederman introduces Noel Weiss, a sprightly 60-year-old retired cop with inoperable liver metastases. “He was hopeless before he met us,” says the doctor in a voice-over, before going on to interview Weiss in an examining room:
Lederman: “It’s been two months since your treatment. What’s happened?”
Weiss: “More energy, great outlook on life. I walked into a cemetery and found an exit marked MARDI GRAS.”
Lederman: “How does body radiosurgery compare to chemotherapy?”
Weiss: “Chemo is like doing a 150-foot bungee jump without the bungee. Body radiosurgery is like having a pleasant dream.”
Lederman, despite his showmanship, is actually a pioneer of sorts. Eight years after he first started performing body radiosurgery, few oncologists would dispute that the image-guided technology he uses will soon be favored over traditional radiation treatment for many types of cancers. But rather than go through clinical trials, with their rigorous protocols, Lederman has opted to take his research directly to the consumer. Tannenbaum, the department’s former head administrator who now has a second career selling real estate in Florida, explains his approach this way: “As a Realtor, we do a lot of marketing. I don’t explain everything in my marketing. My goal is to put enough real information out there to get you interested enough to call. Then, I’ll explain everything in greater detail. The same is true in every other field.”
The details Lederman omitted are significant. Take the claim of 94 percent successful control of primary pancreatic cancer. The statistic comes from an abstract that Lederman published in 2000 about 45 patients he treated for the disease. Curiously, only 17 were evaluated for the study; it was 94 percent of that much smaller group whose cancers were controlled. What happened to the other 28 patients? “Not every patient would agree to send films,” Lederman explains. And when patients die? “If they die, then they don’t send in films,” he says, though he claims that it isn’t only the patients with good results who follow up.
“This is retrospective review,” says Robert Timmerman, a professor of radiation oncology at the University of Texas–Southwestern Medical School who is currently conducting a study of stereotactic radiation therapy for lung and liver cancer. “Retrospective data analysis results in claims of control and survival that have shown to be very different from reality. It’s just so flawed that it’s almost not worth doing.” And what does “control” of pancreatic cancer mean, anyway? “Local control is one thing,” says Albert Koong, a Stanford radiation oncologist who recently published the results of his study on treating pancreatic cancer with stereotactic radiosurgery. “But if you have patients who’ve had the disease spread outside the primary tumor, what’s the point? It’s like slamming the barn door shut after the horse has run out. You can control the tumor locally, but that’s not what’s going to kill you. What’s going to kill you is the metastases, and that’s clearly the role of chemotherapy.”
Lederman doesn’t disagree with this assessment and says he treats metastasized pancreatic cancer to palliate, or reduce the pain of, a patient. He would certainly explain the difference between local and systemic treatment and the vast gulf between local control and cure before he put anybody under the beam. “It’s hard for me to believe that anybody with metastatic cancer truly felt that I was promising a cure.”
In an attempt to show “the other side of Gil Lederman,” the doctor gave me the telephone numbers of dozens of former patients, who all told compelling stories about his kindness, compassion, skill, and how whatever he did with his machine managed to buy their loved ones some valuable extra time on Earth. Noel Weiss, the star of Lederman’s body-radiosurgery video, wasn’t on that list. That optimistic Mardi Gras future of his lasted only weeks after the taping.
“Look,” says Lederman, “just because someone died doesn’t mean they died of the cancer or the treatment.”
I want to see this guy lose his license to practice medicine,” says attorney Matthew Lifflander from behind his cluttered desk. An avuncular 72-year-old, whose round face makes him look a bit like Burgermeister Meisterburger, Lifflander is a different animal from the kind of shiny-suited malpractice lawyers Lederman has encountered in the past. He’s a Ralph Nader type, a former director of the State Assembly’s Medical Practice Task Force who still sees it as his duty to police the medical community.
Lederman first came to Lifflander’s attention when he was asked by Olivia Harrison’s lawyer Paul LiCalsi to assemble her case before the State Board of Professional Medical Conduct. That case may be over, but Lifflander is not nearly done. In June, he filed a $31 million suit in federal court against Lederman, SIUH, and Philip Silverman, another doctor in Lederman’s practice, on behalf of a Florida woman whose husband died after receiving radiosurgery for his pancreatic cancer. “What Lederman is is a greedy ghoul,” says Lifflander. “It’s billing-based medicine.”
Thomas Ryan, a former Brooklyn Public Library employee who’d retired to South Florida, heard about Lederman through his son in New York. He requested a packet from SIUH, which touted a 99 percent success rate for controlling pancreatic cancer. According to the complaint, Silverman told Ryan’s son that he didn’t know whether the treatment would give his dad an additional one or ten years, but that radiosurgery would provide “good quality of life.”
In a last-ditch effort to beat his cancer, Ryan abandoned his circle of friends and comprehensive treatment to come to Staten Island in the spring of 2002. He carried Lederman’s pamphlet with him wherever he went, like a security blanket. According to attorney Richard Reich, who’s working with Lifflander on the case, CT scans from late April show that by the time Silverman was treating Ryan’s pancreas for cancer in May, there were already as many as four clearly identifiable metastases to his liver, which rendered the treatment to the pancreas pointless. By June, his liver looked “like the night sky, with stars,” says Reich. Still, according to the lawyer, Silverman recommended another round of radiosurgery to treat four of what Reich claims were 50 sites of metastasis. “There was no medical reason to treat this man,” Reich says. Ryan died less than a month after his final treatment.
Lifflander is going after Lederman not just for malpractice but for false advertising. He’s taking the novel approach of citing the New York State General Business Law’s statute regarding false and misleading advertising, most commonly used against car dealers who sell lemons. The statute states that if advertisers withhold material information from consumers, they could be held liable for fraud. Lederman’s materials did include wording like “successfully controlled in the treated area,” but if a jury decides that a reasonable consumer interpreted that as a guarantee of a cure or a longer life, Lederman could be in big trouble. And malpractice insurance typically doesn’t cover fraud damages.
Lifflander acknowledges that Ryan was terminal, but he hopes to put a price tag on the last months of a man’s life. “Let’s say you know you have three months to live,” Lifflander says. “Are you going to spend them puking and heaving and pissing in your pants in Staten Island? What’s that worth?”
Lifflander is not the only source of Lederman’s legal troubles. The Staten Island firm of Behrins and Behrins has brought a billion-dollar suit against Lederman and SIUH for, among other things, violating rico, the anti-racketeering statute, by concocting a scheme involving a fake Italian doctor who allegedly received kickbacks for funneling Italian patients to Staten Island using promotional materials that again touted a 90 percent success rate.
Lederman claims that many of the Italian cases he took were palliative only, and a hospital source says the suit is merely the result of a disgruntled former employee riling up the Italian families. But you have to wonder if people who sought only some alleviation of their pain would really travel 4,000 miles for it.
When Federica Losacco Facchini and her husband, Massimo, who at 32 had inoperable liver metastases from colon cancer, traveled from Bologna to Staten Island in 2002, they were coming for a cure. “Without question, the thing that first attracted us was the 90 percent success rate,” she says. “It said that it would cure tumors that had metastasized. Nobody ever said that. Who wouldn’t call? It’s unquestionable that what they’re offering you is a miracle cure. They don’t use that word, but that’s what they were promising.”
Back in Italy after the treatment, Massimo started running a high fever. When Federica called the hospital, she says, she was told by an Italian-speaking program aide, “It’s better he has a fever. It means the body is eliminating the tumor.” Four and a half months later, he was dead. According to Facchini, all ten of the patients who were staying at the hospital’s residence hall when she and her husband were there had metastatic cancer. Not one is alive today. “How can you say you have a 90 percent success rate if no one survived?” she asks.
It may not be fair to blame Lederman for the deaths of his terminal patients, but what if his treatment increased rather than palliated the pain they experienced in the last weeks of their lives? That’s what attorney Steven North says happened to Suzanne Mikul, a 68-year-old preacher’s wife from New Mexico who died from colon cancer. After being diagnosed in 1996, she had a colostomy, a harrowing round of chemotherapy, and three courses of standard radiation. Her doctors told her that her body, after receiving a lifetime total of 9,560 rads, just wouldn’t be able to take any more radiation exposure.
“We were praying for supernatural healing,” says her husband, John. “But as far as medicine, there didn’t seem to be anything else we could do for her until we heard about this treatment.” He says that when they arrived in Staten Island in November 2001, they were assured by Silverman that SIUH’s radiation wouldn’t count against the radiation totals Suzanne had previously received. “He didn’t give any guarantees, but there certainly weren’t any warnings,” says John. (Silverman could not be reached for comment; Lederman’s attorney declined to address the case.)
After receiving 3,000 more rads, Suzanne went home and waited for her tumor to shrink or disappear. Soon she started feeling pain in her lower back, and nurses noticed that what had started as two patches of redness had scabbed over and looked infected. A surgeon was called in to debride, or scrape away, the infected tissue. The surgeon scraped and scraped and made an alarming discovery: In two softball-size areas above her buttocks, all that was left between Suzanne Mikul’s skin and her abdominal cavity was liquefied dead flesh. By the time he finished cleaning the wounds, he could see clear through to her tailbone and down into her exposed gut. Stool and undigested pills were leaking right out of the holes in her back.
“Do you have a strong stomach?” asks North as he passes a five-by-seven color photo across his desk. It looks as though she’d been shot at point-blank range with a double-barrel cannon.
These days, Lederman, who seems hell-bent on not expressing the slightest bit of contrition about anything that’s happened, is pursuing the defiant course of doing precisely everything that got him into this mess in the first place. In March of last year, he was hired by the cash-strapped Cabrini Medical Center, which chose to overlook the potential public-relations nightmare and focus on the business he might bring in. (To help his case for employment, Lederman managed to produce George Harrison’s only—though virtually estranged—sister to vouch for him with the Cabrini CEO.) Since then, traffic through the radiation-oncology department has doubled, and the hospital is looking for space to install a new linear accelerator. Lederman’s celebrity pictures are up on the walls. He recently met with a Lederman club in Italy. And he’s producing numbers-heavy brochures. His practice would certainly be sending out videos by now, if it weren’t for that pesky coot Lifflander, who scared the Cabrini administration into shelving his first one by claiming that the use of patient testimonials is illegal under state law. Lederman’s got a plan to remedy that problem.
Three days before Thanksgiving, Lederman is sitting in the sixteenth-floor Cabrini lunch room, which has been converted into a reasonable facsimile of the Charlie Rose set, complete with round table, black backdrop, video cameras, and TV lights. Across the table from him is a knockout brunette named Tahna Regan-Fischer, the sister of a former patient. She’s been flown in from Phoenix to play the inquisitive, pretty young woman you always see in infomercials, because the law doesn’t say anything about sisters of patients declaring that Lederman is a wonderful doctor.
Her brother, Todd, suffered from meta-static hemangioperisitoma, a rare soft-tissue sarcoma that spread to nine inoperable sites in his body. Regan-Fischer encouraged him to see Lederman after she read a George Harrison obituary. Todd died last January. “The next to the last thing my brother ever said to me,” Regan-Fischer told me a few weeks before the taping, “was that he thought Dr. Lederman was a great guy.”
After she applies her hair spray, the room falls silent and the twin cameras start rolling. Lederman poses a question, some version of which he’ll soon have to address in court. “There’s a delicate line for a physician to be too reluctant to offer treatment or too eager to offer treatment,” he says. “How do you think my relationship was towards Todd?”
“Most people were telling him, ‘You need to do this, you can’t do that, you’re going to die. This is going to work. This is not going to work. Try this. You’re going to lose your hair. You’re going to vomit,’ ” she says placidly into the camera. “You didn’t say anything like that. You said this is what you have. This is what we can do. And it worked.”