Last month, a new type of intrauterine device, or IUD, called Kyleena joined the other four on the market. Lots of women love their IUD because it’s a set-it-and-forget-it method that’s more than 99 percent effective at preventing pregnancy, which lasts for years but that you can have a doctor remove at any time. So which one is best for you?
The five kinds all work roughly the same way: They thicken cervical mucus so sperm can’t enter the uterus to fertilize an egg. In the rare event that some mighty swimmers do get past the cervix, the IUD’s active ingredient (either copper or synthetic progesterone) makes it more difficult for them to travel through the uterus and tubes toward an egg.
Insertion is the same with all of them: not comfortable, exactly, but usually manageable. But the devices have different amounts of hormones — or none at all — and will change your periods in different ways. Among the hormonal IUDs, the higher the hormone amount, the more likely it is that your period will stop after six months to a year. Here’s how they compare to each other.
ParaGard
Best for: Women who want to avoid hormones.
Skip if: You have heavy periods.
The Old Faithful of IUDs, ParaGard is a non-hormonal option where copper
acts as the sperm deterrent. It’s approved for ten years, but studies
say it’s actually effective for 12.
Some women love the idea of birth control without hormones, but if you
have naturally heavy periods or if your doctor says you have
endometriosis, getting a copper IUD might make an already bad situation
worse.
Keep in mind, too, that you might not remember what your period is like sans hormones if, say, you’ve been on the pill for a decade,
says Laura MacIsaac, MD, MPH, FACOG, director of family planning at
Mount Sinai Health Systems and associate professor of obstetrics and
gynecology at the Icahn School of Medicine. “The first three periods
after a new ParaGard insertion can be … pretty bad. Just heavier and
crampier. And then, [with] most women, their period gets back to their
baseline,” Dr. MacIsaac says. But she points out that a heavy flow
doesn’t happen to every woman — some might not notice a difference.
Mirena
Best for: Women with heavy periods.
Skip if: You don’t want your period to disappear entirely.
Mirena was initially approved for women who’d already had children, but
that’s just because those were the women recruited for the study
submitted to the FDA. Doctors prescribe it to women without kids all the
time and, in fact, the American College of Obstetricians and
Gynecologists has recommended long-acting reversible contraception as
the first-line method for adolescents since 2012.
Where ParaGard can make periods worse, a hormonal IUD could help improve
painful periods — in fact, Mirena is also FDA-approved for the treatment
of heavy menstrual bleeding, or menorrhagia. About 20 percent
of women with a Mirena see their period stop after a year, as do a
third of women who use it longer. Mirena is approved for five years but
recent data says it’s effective for seven.
Liletta
Best for: Women on a budget.
Skip if: You don’t want your period to disappear entirely.
This device is a pharmacologic equivalent to Mirena (it has the same
total amount of hormones), but was developed to be less expensive for
women visiting family planning clinics who are either on Medicaid or lack health insurance. It costs providers $50
and they can pass on savings to their patients. It’s not technically a
generic because it looks a little different and releases slightly less
hormone on a daily basis, though there is the same amount of hormone in
the device. Still, about the same number of women reported amenorrhea
(no periods) with Liletta as with Mirena (Liletta’s rate is slightly
higher after three years).
It’s currently approved for three years but the manufacturer will be submitting five-year data to the FDA and will continue to study
the same group of women for seven years. It’s possible that Liletta could
last even longer than Mirena since the daily release is lower, but only
further research can prove that.
Skyla
Best for: Women who like the idea of a smaller IUD.
Skip if: You’re looking for a long-term commitment.
This device is approved for three years and is specifically marketed to
women who haven’t had kids. It’s smaller than Mirena, which makes it
more appealing to people who haven’t had their cervix dilated, but we’re
talking about the difference of a few millimeters, says Kristyn Brandi,
MD, family planning fellow at Boston Medical Center.
What is different is that it releases fewer hormones on a daily basis,
meaning more women keep getting their periods on Skyla versus with
Mirena — which is appealing if you would prefer to keep your normal bodily
function intact, Dr. Brandi says. (Only about 6 percent of Skyla users stop getting their period after one year; 12 percent of users stop after three years.) That, and it’s only approved for three years. If
you want contraception for longer, you should probably get a different
IUD.
Kyleena
Best for: Women who want more than three years of use, and want to keep menstruating.
Skip if: You don’t have the patience to fight with your insurance.
Bayer, which manufactures Mirena and Skyla, developed this newest IUD which became available in October. Kyleena is approved for use in women regardless of whether they’ve had kids. It releases fewer hormones than Mirena, but more than Skyla, though it lasts the same amount of time as Mirena.
This device might be a better option for women who want five years of pregnancy prevention but would rather get their period than not. In the approval studies, about 12 percent of women stopped getting their periods after one year, and 20 percent did after three years. But beware: If you’re interested in Kyleena, it could be a hassle to get your insurance to pay for it for the next five to six months until the temporary billing code designated for new drugs and devices becomes a permanent one, Dr. MacIsaac says.
Here’s a handy chart with the dosing and approval length for each IUD.
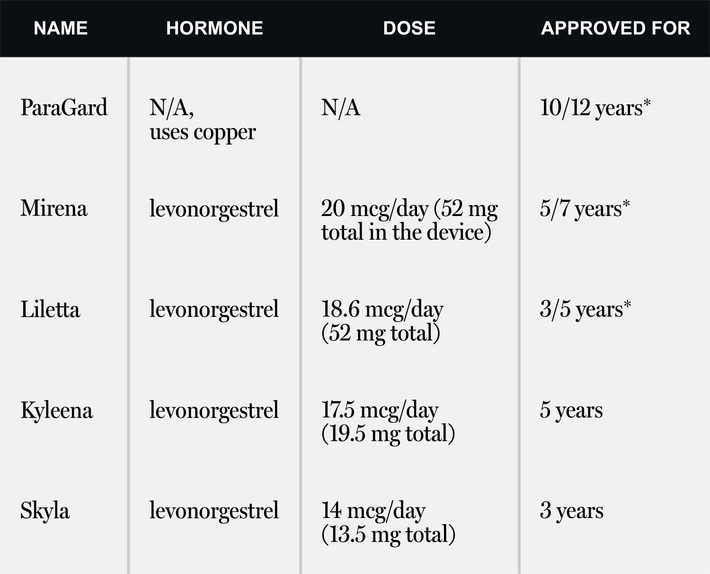
*Additional studies show that the devices are effective even longer than originally approved for: 12 years for ParaGard, seven years for Mirena, and five years for Liletta.




