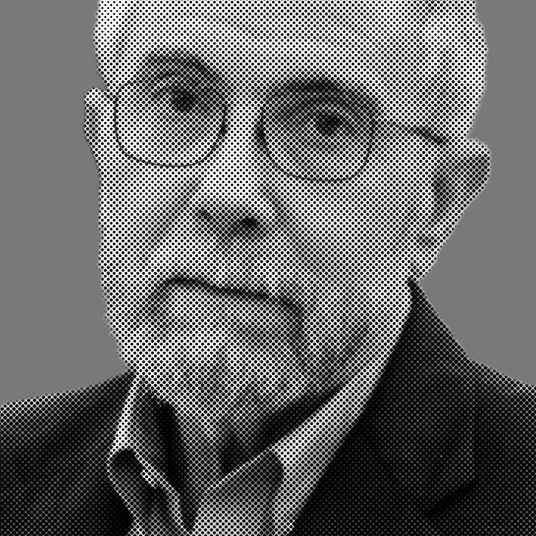
Japan’s Prime Minister Shinzo Abe is reportedly considering fast-tracking antiviral remdesivir for use on COVID-19, despite the treatment’s failure to show that it works in clinical trials. Should Abe go through with it, Japan would become the first country to approve remdesivir for use. Experimental vaccines as well may be approved for emergency use in the near future, which is not unprecedented. As a clinician working on the Ebola outbreak on the border of Uganda and the Democratic Republic of Congo in 2018, Dr. Nahid Bhadelia was injected with an experimental vaccine which was going through an open-label trial, but had not yet been approved by the FDA. Intelligencer spoke to Dr. Bhadelia, who is the medical director of the Special Pathogens Unit at Boston University’s National Emerging Infectious Diseases Laboratories, about remdesivir, New York City’s plan for contact tracing, and the vaccine treatment she is most optimistic about.
Mayor de Blasio just announced the city will hire 1,000 people to do contact tracing that will begin in May. What will that program look like on the ground?
Ending this thing isn’t just about bringing in the sick people. What it will take is the simple, iterative process through which you find someone who’s sick, and then you find everybody else who they would have been around during the period of time that they were contagious, and you ask them to quarantine themselves until they develop potential symptoms or until they’re out of the danger of developing symptoms. What you’re doing is breaking something called chains of transmission. That is particularly important for a disease like COVID-19 because it’s actually much, much easier to transmit than Ebola, where you need contact with the bodily fluids and need to be very close. With COVID-19, it’s respiratory, and all it takes is spending 10 minutes within six feet without any protection.
Contact tracing seems like it could have been critical in early February. Why is it important now, when New York City is on the other side of the curve?
It’s actually almost the other way around. If there are tons of cases everywhere, there’s just not enough manpower to do that kind of contract tracing. That’s why you need a blunt instrument, like the public-health restriction measures, to block chains of transmission. Now that the cases are dropping, we have a bit more capacity to actually build up the manpower that could trace new chains of transmissions that are occurring as we’re thinking about opening up more segments of society.
A new report from health-news site STAT and Harvard says that many states aren’t doing nearly enough testing to reopen. What I don’t really understand is how this could be a state-by-state process and not regional or nationwide. Isn’t Georgia affecting Florida and Alabama?
It needs to be both. States need to plan according to the capacity of their health-care systems. We should learn from the experiences of New York and Boston and other cities. Things are pretty dire still. Our CEO at the Boston Medical Center mentioned that more than 70 percent of our cases are COVID patients. Thankfully, no Massachusetts hospital has reached a crisis standard of care — they didn’t have to make hard decisions about resource utilization and distribution. But we’re still at really high levels. When cases are dropping, as they are in New York, the concern for any state is that, for every set of new infections, there is a portion of those infections that will end up in the hospital. We know from serological studies — all of the caveats about effectiveness of those tests aside — we have nowhere near the kind of immunity that you need to open up society without a portion of people ending up in the hospital.
The first question for all of these states is, if you get clusters of cases, are you ready to take care of them? The second is, how do we actually stop those cases from happening? That takes state resources to develop contact tracing and case finding. So it is a state-resource assessment, but it is everybody’s problem if Georgia’s outbreak goes out of bounds, because we will all be affected with new cases. The Delta hub is in Georgia! Everybody flies out of that airport.
The latest antibody figure in New York City shows 25 percent of people testing positive for antibodies. What can we do with one-quarter of the nation’s largest city walking around with antibodies?
That’s still not the number we need. There’s an equation one goes by to figure out what herd immunity is for a particular disease. That’s the function of the R0 and other variables that I won’t get into. Hearing [infectious-disease epidemiologist] Michael Osterholm talk about it, 60 to 70 percent is the kind of number we need to actually say that we have herd immunity. So whatever this opening looks like, whenever it happens, it needs to happen with caution. It certainly will not be the normal that we knew.
Another element that I think is important: Getting a better handle on how many people have already been infected will give us a sense of how many people are transmitting asymptomatically. We kind of already know that from some studies, which have shown that about 40 percent of transmissions happen in the pre-symptomatic or asymptomatic period. That’s from one small study. Getting a population for how many transmissions are happening, and at what rate, will give us a better handle on what the public-health interventions should be. Maybe we need to think beyond contact tracing to other innovations, like employee surveillance and protection, decontamination, and greater distancing between people in public spaces.
What are you following closest right now in vaccine news?
Last I checked, there were six vaccine candidates at phase-one trials. U.S.-based companies have two: Moderna is doing the RNA-based vaccine, and Inovio is doing the DNA-based vaccine. There are three now from China, including one that showed pretty good promise in animal models that I saw the results of at the end of last week. And there is one in Oxford, which uses a platform that reviews for other diseases called chimp adenoviruses. The lag time for figuring out if vaccines work or not is because you have to see their efficacy in animal models before you take them into healthy humans, which is phase one. The phase-two and phase-three trials are meant to show you efficacy, because you’re vaccinating a certain portion of the population and not vaccinating another portion — you’re letting natural infections happen. That gives you an idea of whether or not it’s safe in a larger group of people, because it’s bigger than the phase-one trials and it gives you a sense over time if they are at a greater or lesser risk than the control arm of this disease. That’s what takes time.
I think you’re going to see multiple vaccines move on to the next phase. That was the case with Ebola. In that case, an emergency vaccine was deployed before it was FDA approved. It was the middle of a crisis in the Democratic Republic of Congo and Uganda and elsewhere. I got that vaccine because I was volunteering on the border of Uganda and DRC. It was not FDA approved, but it had gone through a phase-three trial already in Guinea. As people talk about emergency deployment, I think you still need a certain amount of human data to feel comfortable deploying it in the emergency setting.
It looks as if Japan is considering deploying remdesivir before the U.S. has approved it. Could that provide the sort of human data that moves it closer to use in the U.S.?
I think it’s worth going into what viral diseases generally do. Viral diseases are generally a one-two hit on your body. The first hit is basically the damage the virus itself does to the body. The second wreaks havoc on your immune system and activates your immune system in an uncontrolled fashion, in such a way that your own soldiers are attacking your body. The secondary damage of inflammation comes from that. You have to think about those two phases as you think about what might work in those scenarios. One presumes that most of the antivirals will work if you’re early enough in the disease — once you have the virus but its level is not very high.
I say this because we’ve had these conversations in the press about whether or not the remdesivir trial is going to be successful. There are signals now that say it’s not going to be successful in severely ill patients, but we still have to wait and see what the data is going to be for moderately ill patients. That’s going to be important data. And what will that mean for the U.S.? If we don’t have enough doses, it won’t matter; it’s a downstream problem.
Anything else you’re following closely this week?
You might have seen there’s an interim French study that just came out on tocilizumab, which is a drug that’s used in autoimmune diseases, an IL-6 blocker — it calms down your immune system. It’s something that is going into trials. The French trial that just came out is a randomized-control trial that shows efficacy. I haven’t seen the data itself, but it was 65 patients in placebo and 65 patients in tocilizumab, and it showed improvement in people who got tocilizumab. We’re just starting a trial on it at Boston Medical Center, and other places have been doing trials on it as well.
The thing I’m really holding out for is a whole other class of drugs that I think will move forward: monoclonal antibodies. With Ebola, there was a four-armed study in DRC that compared an antiviral, which is remdesivir, against three monoclonal antibodies. With monoclonals, you look at a survivor’s body, you take their blood, you find those antibodies that are very good at blocking virus activity, and then you clone those antibodies and try them out in animals and humans. Monoclonal antibodies ended up being the most successful therapy in Ebola because they serve this function of blocking all viral activity earlier or later in disease.
On Thursday, there was a study from China that showed that they have identified two very effective monoclonal antibodies. It was just bloodwork. Nothing else has been done — it hasn’t been tested in animals, hasn’t been tested in humans. But Regeneron, a company that has been working on other things, is working on a model for those monoclonal antibodies, and there might be other companies that pick it up. I’m hoping that is the third kind of treatment, aside from convalescent plasma, that will provide some answers. We have a long way to go on that, though.