For thousands of Americans, a coronavirus diagnosis was only the beginning. For months now, people who recovered from the initial illness have been experiencing a wide range of persistent symptoms: shortness of breath, weakness, brain fog, fatigue, depression. Countries hit hard by the pandemic in Europe have begun offering rehabilitation services to COVID-19 survivors, but the medical science community still knows very little about how the body recovers from the virus’ attacks on the lungs, gastrointestinal tract, heart, kidneys, liver, brain, and nervous system.
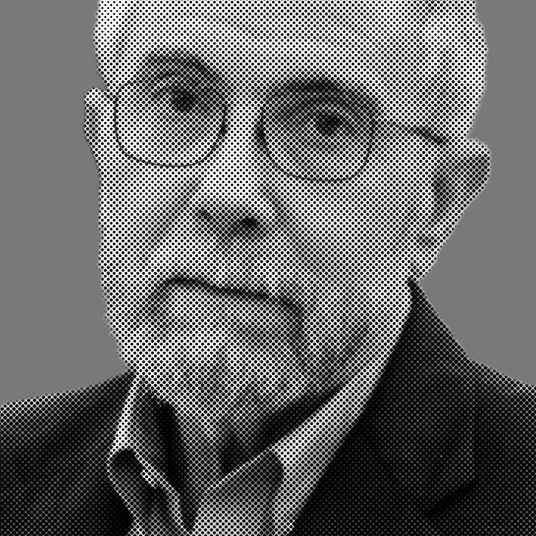
“This illness is more than just the initial infection, and to get a handle on it, we needed to learn about it,” says Dr. Zijian Chen, medical director of Mount Sinai’s Center for Post-COVID Care, one of the first places dedicated to treating people reporting long-term coronavirus effects. Since opening in May, the center has seen 300 patients who were either COVID-19-positive or presumed positive, and have continued to experience distress. Intelligencer spoke with Dr. Chen about the wide range of symptoms he’s seeing, the psychological toll of COVID-19’s aftereffects, and his fear that some patients may never recover.
It’s been a little over two months since you opened this post COVID-19 care center. What have you learned?
That recovery is going to be a very long process for many people. We’ve been seeing patients for two months. And we’re at the beginning stages of learning exactly what types of symptoms COVID patients will have long-term. The more patients we see, the more types of symptoms we’re finding out about. Over time, I think we’re going to find ways to treat all of these symptoms, but that’s going to be a very long process.
One study out of Italy reported nearly 90 percent of patients recovering from coronavirus were feeling symptoms two months after the virus was detectable. What sorts of numbers are you seeing?
It’s very, very close to that. Everybody we see has symptoms. Because of that, I can’t tell you what percentage of people infected will have symptoms and what percentage will not, but these are not just patients who had been hospitalized. These are patients who got sick and were home but continue to have symptoms that are unrelenting. I feel like the population of this is going to be very large.
What percentage of the patients you are seeing were hospitalized?
Not that high. Maybe 20 or 30 percent.
What’s the range of symptoms?
The most prominent of these symptoms is definitely shortness of breath. I would say 60 to 70 percent of our patients are short of breath in one way or the other. Then there is chest pain and chest discomfort, and then neurological symptoms, like fatigue, weakness, poor concentration, poor memory.
What’s the most surprising symptom you’ve seen?
The most surprising thing I’ve seen is how much psychiatric illness there is — anxiety and depression. There’s a very high percentage of that.
Is that anxiety from the experience of having COVID or from the frustration of not knowing how long the symptoms are going to last?
I think it’s a combination of the two. Both of those are very traumatic events. Not only are patients ailing with that initial illness, they now have something that’s really persistent, and has been for months. They don’t know what to do because, unfortunately, some doctors don’t believe that they really have these symptoms and the doctors who do don’t have resources to get help. All of this combined is very stressful.
Are you diagnosing patients with PTSD?
I would say anywhere from 25 to 35 percent of the patients we see are suffering from anxiety, depression, PTSD, or something similar.
Is there a link between the psychological toll and the physical ailments?
Not directly. We haven’t started compiling the data yet, but I would imagine the more residual post-COVID symptoms you have, the more likely you are to have some psychiatric effects.
For patients who have, say, shortness of breath, have you witnessed any improvement after they come to you?
Some have improvement and others are still at baseline, meaning they haven’t improved. What we do is pull together a team of cardiologists, pulmonologists, and rehab doctors. They give the patient medications to help them breathe better, whether it be medicine that opens your airways or decreases inflammation. If that doesn’t work, we help patients condition themselves so that their bodies are better prepared to exercise. That helps with overall muscle function and breathing. We’re seeing whether this cooperative approach between different specialties can help, rather than just having one specialist see the patient.
In terms of the lasting symptoms you’re witnessing, what can you compare this disease to?
That’s an interesting question. COVID is unique in that there are so many different body symptoms. I can’t really think of another illness that’s as traumatic. You have some autoimmune diseases that may be similar, but one thing that stands out is post-ICU syndrome. There are patients who suffer acute illness — they’re in the ICU for a very long time. From there, they’re discharged after they get better, and have residual symptoms for a long time because of the de-conditioning or possible super infections that happen in the ICU and also the effect of, say, sepsis or whatever illness that put them there. But we’re seeing this in patients who weren’t hospitalized.
What are you most concerned about?
I’m most concerned about how very little we know about the symptoms and the expectancy of how long they will last. If you look at the total cases, even if a small percentage have these post-COVID problems, we’re going to be in a lot of trouble. That would be an immense number of patients. Our health system cannot take care of that many people.
Have you been able to nail down an average recovery time for any of these symptoms?
No. I wish we could. That’s the uncertainty. We’re still on the upswing of this curve. The more people who get sick and recover from the initial illness, the more people will start to develop these secondary symptoms. We don’t even know when we’re going to hit that peak of chronic patients. Looking at the data, some of the damage may be permanent. Permanent lung fibrosis and similar damage to other organ systems.
I think a lot of the pulmonary symptoms are going to be very long-lasting. That’s the best data we have right now. We know that there’s a lot of pulmonary damage beyond just the viral infection. We know there’s a lot of immune system damage that happens during the infection that damages tissue in the lungs so badly that it’s no longer functioning. That’s why the patients have shortness of breath, because part of their lung tissue just isn’t working. It’s very similar to very acute bacterial infections that also destroy lung tissue, and patients don’t fully recover after that. I can imagine many patients will have shortness of breath for months or years, if not the rest of their lives.
This interview has been edited for length and clarity.