On Sunday, President Trump’s doctor said that the president has been given dexamethasone, a steroid treatment used to help severely ill patients with COVID-19. The disclosure conflicted with the White House’s previous statements that projected a far more optimistic picture of the president’s health. It also raised questions about the potential side effects of steroids, including “grandiose delusions,” which Trump did little to allay Monday morning when he rattled off a long series of tweets that were almost lyrical in their simplicity. “PRO-LIFE! VOTE!,” “SPACE FORCE. VOTE!,” “BETTER & CHEAPER HEALTHCARE. VOTE!”
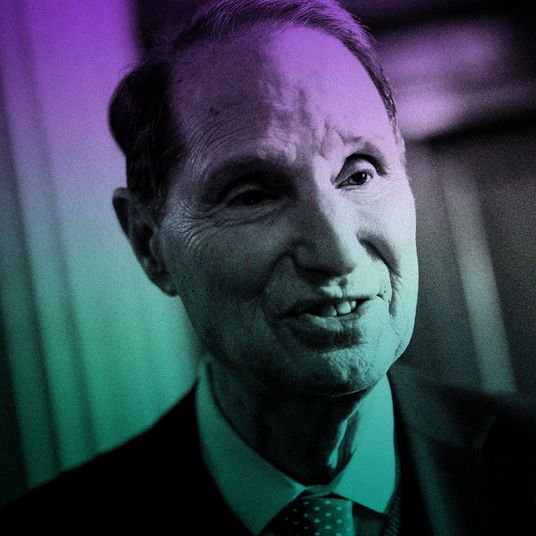
Dr. Bryan McVerry is a pulmonologist and an associate professor at the University of Pittsburgh Medical Center, as well as the co-author of a recent study that showed how steroid treatment improved survival in very ill COVID-19 patients. Intelligencer spoke to McVerry about the president’s treatment, the side effects of dexamethasone, and whether the president would have been treated with steroids had he not been severely ill.
From what little we know about the president’s health, what do you make of the fact that his doctors administered steroids to treat COVID-19?
The data supports the use of steroids in patients with more severe clinical manifestations of COVID-19 pneumonia — people who have oxygen requirements or people who require respiratory support in the form of mechanical ventilation in the intensive care unit — as the ones who derive the most benefit out of steroid administration. The information that has been available to me as part of the public has suggested that the president’s course has been relatively mild in terms of its progress but perhaps there was more to the story. I know one of the physicians on the treating team and I know him to be a good doctor who carefully weighs the evidence in making the decisions that he makes around treatment of his patients. And so I trust that the doctors taking care of the president felt that the treatment was indicated and gave it appropriately with their clinical judgment. I just haven’t seen the evidence myself that he had more severe disease.
What do you mean when you say severe clinical cases?
Our patient population in the REMAP-CAP COVID steroid trial were all patients in an intensive care unit receiving organ support defined by mechanical ventilation, noninvasive mechanical ventilation, or pressure medications to support their blood pressure. Other hospitalized patients are characterized as either requiring oxygen support or not, basically. So the more severe patients who I’m talking about are patients who have pneumonia from COVID-19 and require oxygen as part of their treatment plan, or require intensive care unit provision as part of their treatment plan. Some patients will get admitted to the hospital with either mild pneumonia, where they don’t need oxygen, or other manifestations of COVID-19 like gastrointestinal disease with diarrhea. They may be short of breath, but not need oxygen.
Is there any reason to administer steroids to a patient who isn’t a severe case?
I don’t think so. I don’t think that steroids are a preventive treatment in terms of progression of COVID-19 and if you look at the data from the recovery trial, which was the study published out of the U.K. in September, that was sort of the first steroid paper, a dexamethasone study, in patients with less severe disease, there was no clinical benefit, and potentially a trend towards worse clinical outcomes in patients who got it with milder disease. That didn’t reach statistical significance, but the odds ratio was headed in the wrong direction with the patients that they had recruited. I’m not sure you can draw any real conclusions from that except to say but there was no benefit — at least no trend towards benefit — on the population.
The treatment of infectious diseases with steroids is a little bit complicated because the infection can cause injury. The host response to infection can cause tissue injury. You may need the host response to infection to fight the infection initially, but it may cause complications of illness downstream, and so the timing of steroids administration may actually determine its relative risk-benefit ratio.
Can you describe what steroids do for COVID patients?
I don’t know that the absolute mechanism of action of how steroids are protective has been worked out. That being said, steroids have long been used as immunosuppressant medications in inflammatory diseases like rheumatoid arthritis or lupus or something of that nature. Steroids have been used in asthma. Steroids have been a long-standing interest in acute illnesses like sepsis or acute lung injury, as a potential disease-modifying agent because of the profound host inflammatory response that drives some of the organ injury in those critical-illness syndromes. I think the theory behind how steroids might be helpful in more severe COVID-19 is that temporizing the host immune response may lessen the organ injury associated with the viral infection, because the organ injury may be related to the host inflammatory response to the virus, in part, in addition to the viral infection itself.
What would be the protocol? How often would you administer steroids?
The trials were sort of relatively low dose for a fixed duration over a period of time. The dexamethasone study in a recovery trial was six milligrams a day for ten days, or up to ten days. The REMAP-CAP COVID steroid trial was hydrocortisone administered four times a day for seven days, or until hospital discharge, whichever came first. Usually it would be not just a onetime dose but it would be a daily dose for a period of time. That period of time would be defined by the amount of time spent in the hospital, at least in the context of those trials, so would not be continued necessarily after discharge from the hospital in those contexts, at least in those trials.
But the president wouldn’t need to be at Walter Reed to continue, he could receive steroid injections at the White House.
I think it’s a question of indication for steroids. In my mind, the indication for steroids is treating patients with more severe respiratory manifestations of the disease — requiring oxygen or requiring intensive care unit support. If a patient, regardless of who that patient is, were being discharged from the hospital and didn’t require oxygen as part of their treatment plan, then my sense would be that steroids would no longer be indicated and would not provide additional benefit. I’m not involved in the treatment team of President Trump and I’m not involved in taking care of him outside the hospital, it may be that he warrants further treatment with steroids. I would defer to the team taking care of him to make that decision. But from my perspective, if you’re discharged from the hospital and you don’t require oxygen anymore, the indication for steroids goes away.
What sorts of side effects are to be expected?
The side effects of steroids are variable. People can feel sort of increased appetite and increased energy with high doses of steroids, they can have elevations in their blood sugar in relation to high-dose steroids. There’s an immune-system suppression that comes with being on steroids, so they can be more susceptible to other bacterial or opportunistic infections. When you use them long term they have more consequences related to bone-density loss and things like that, but in the short courses they tend not to have those lasting side effects that other people might see if they use it long term.
People have described some extreme, maniacal side effects. How much variation is there?
That’s why I said people can have this sort of increased energy being on higher doses of steroids. I’m not sure I would liken it to any other sort of syndrome necessarily, but you can get sort of activated and jittery by taking high doses of steroids for a short period of time. It’s not uncommon for people to have restless sleep, increased appetite, increased levels of energy, maybe could be a little bit tremulous if you take super-high doses, but the doses that we typically use for COVID-19 are not that high. But people could have manifestations of increased energy.
Looking at his tweetstorm today — which, even for the president, seems like erratic behavior — do you look at that and say that this is because of steroids?
I have to confess that I have not followed his tweetstorm today. But hearing some people talk about it, getting doses of steroids can certainly sort of activate you and energize you, so to the extent that he’s feeling better and activated and energized as a result of that, I suppose it’s possible.
Are there recommendations for patients about behavior or what they should or should not be doing, or should be avoiding once they’ve been given steroids.
Not necessarily. Depending on how high a dose and for what period of time, you may give some prophylaxis against other infections, but for these short courses of steroids that we’re talking about in COVID-19, there’s no real particular recommendations in that regard.
Knowing that the president was given steroids over the past few days and he’s leaving the hospital tonight, is that a short recovery period or is that typical?
I think every patient responds differently with the infection so I’m not sure you could necessarily say that there’s a typical course or typical timeline of recovery for patients as a whole. The people with more severe disease end up staying in the hospital longer, I think that makes intuitive sense.
With what we actually know around the president’s case it’s hard to speculate as to how quickly we might expect him to recover. Usually people with COVID-19, people manifest more severe complications of the disease typically seven to ten days into the evolution of the syndrome, but everybody responds differently. He seems to be on the mend, which is a good thing, and from what we can see from the news reports, he seems to have a relatively mild course of illness, which is also good for him, but it’s hard to know without being there and being part of the treatment team exactly what they’re dealing with.
Can steroids mask symptoms in COVID-19 patients? Like a cortisone shot for an athlete.
That’s a hard question to answer. I mean, certainly you would not mount a fever response necessarily on the doses of steroids, so you might mask the development of fever, but I’m not sure that the sort of increased level of energy that you would get from steroids would necessarily mask the progression of disease. I think it’s very different from a cortisone shot into a joint, which suppresses the inflammation in that joint and alleviates the pain locally. That’s a different sort of treatment process than giving systemic steroids for a disease such as COVID, so I’m not sure you can draw that corollary. I don’t think you would miraculously look better while you are otherwise getting sicker in the context of the doses of steroids that we’re talking about.
So no Weekend at Bernie’s type of situation.
I’m not sure we should get into conspiracy theories on how things are happening in the president’s course of illness. I think we need to stick to what we know and what we know about the disease and what we know about the treatments. We have to assume that the people taking care of him are qualified people who are doing what they think is in his best interest as a patient. There’s no magic to being hospitalized with COVID-19. You can be home with COVID-19 as long as your manifestations are relatively mild. You can be monitored outside the hospital, so if he’s gotten to a point where the treating team thinks it’s reasonable for him to convalesce at home, I don’t think it’s unreasonable to discharge him.