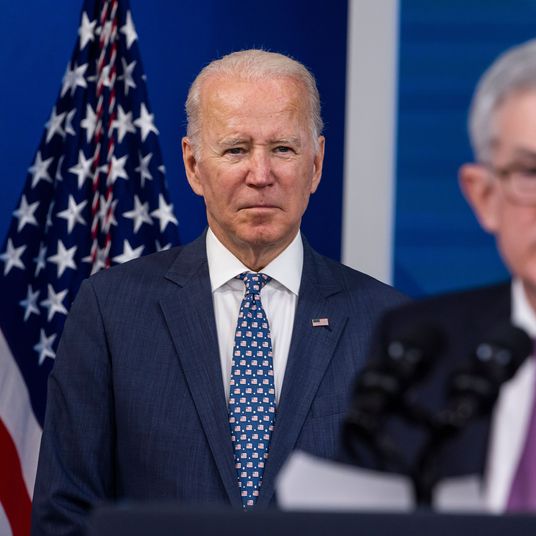
Last spring, Dr. Michael Osterholm doubled down on his reputation as COVID’s Dr. Doom and warned that the darkest days of the pandemic still lay ahead, despite vaccination, due to the emergence of new variants. A few months later, his prediction came true with Delta, which has killed more than 100,000 in the U.S. alone. Now Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, is eyeing Omicron. Intelligencer asked Osterholm how Delta will fare against the new variant, how worried we should be about lab tests showing immune escape, and whether the term fully vaccinated should continue to apply to the unboosted.
You rustled a lot of feathers in April when you talked about the threat of the coming variant waves. We’ve really gone through it with Delta, and there are a lot of concerns about Omicron. How many more times can you ring that bell?
I don’t think I have to anymore. The world has come to understand what the variants can do. My line, which actually is more true than you’d believe, is that back in August I’d wake up in the morning humming this song by the 5th Dimension, “This is the dawning of the Age of Aquarius.” But I’d be singing, “This is the dawning of the Age of the Variants.” I had every reason to believe we were going to continue to see variant development because we had more and more transmission. What biological pressure, or what evolutionary law, says that with more transmission we’d have less variance, not more? It made no sense. Eventually, there was no reason anything would replace Alpha unless it was more infectious. And that’s what has happened with Delta, and now we have Omicron. Three weeks ago, just before the first cases in South Africa, I said Delta is here now, but I worry about the next variant that’s going to be coming.
Delta has overwhelmed the country. Is that the wave you were predicting when you said we had dark days ahead?
Yes, that’s what I meant last April when I said potentially some of the darkest days of the pandemic are ahead of us. I came about my point of view in March or April with Alpha, and then Beta and Gamma, and said we were a long ways from being done with these. So I thought Delta was really not a surprise. I had come to the conclusion that the next variant would be much more transmissible. That was probably going to be the key factor in crowning the King of the Virus Hill. Sure enough, that was the case with Delta. Since then, I’ve said that anything that’s going to knock off Delta is going to be even more transmissible.
Here in Minnesota, we’ve had a surge going on since August. This is remarkable. Most of the country has missed the fact that there have been these two different patterns of surges: One I call the India surge pattern, where cases rise quickly, hit a high peak, and come down relatively quickly back to baseline; then you have the U.K. model, where basically, in July there were 1,500 cases a day, then it went all the way up to 53,000 cases a day, then came down at the end of July and early August to 23,000 cases, and then it went right back up again. The U.K. has been in a major surge since July. We’ve also been in a major surge in Minnesota. The epi curve started to pick up in August and never really came down. We don’t understand why these different surges occur. No one can tell you why a surge starts or stops — and be careful if they do because they probably have a bridge to sell you. We just don’t know. We do know that vaccination and previous immunity can have a big impact on the height of these curves. But why do they start or stop? I don’t know. That’s part of the humility with this virus that is so critical.
As far as long-term impact, at what point will a variant’s severity of illness be a bigger factor than its transmissibility?
We’re actually in a very critical moment in this whole pandemic. What is going to happen in the battle between Delta and Omicron? That is going to be key. Will Omicron beat out Delta, just like Delta did all of the previous variants before that? With the information we’ve seen to date, that is surely a real possibility.
Now we’re at this point where we may have the highly infectious Delta, which surely is causing very serious illness and deaths, up against one that is likely much more infectious and transmissible, and at the same time all of our early evidence suggests it may cause much less severe illness. Would it be an ironic situation if, in fact, Mother Nature herself helps us out of this pandemic?
Much of the coverage of Omicron right now is fixed on relatively small lab studies of vaccine evasion. Isn’t what’s happening on the ground in hospitals in southern Africa more important at this point?
That’s what I’m looking at. Last weekend, I said I’ve been impressed by two things. One, how transmissible this is, not just in South Africa but around the world. Look at outbreaks in Oslo, Spain, Denmark, and the U.K.; clearly, they all mark a substantially increased transmissible virus. But the second thing was, even when trying to understand what was happening in South Africa or elsewhere, we just haven’t seen a developing wave of severe illness — which isn’t to say it can’t happen or won’t happen. I’ve been one of those people out there talking about lagging indicators and how important they are to understand that severe illness, hospitalization, and death often occur two-to-four weeks after cases. So we need to be very careful about that. But here I am four or five days after saying that, and the data are still, I think, generally speaking, showing less severe illness.
What will that mean for a U.S. population that’s still only 60 percent vaccinated?
That’s what’s going to be really important to understand — that third piece, immunization. What does that mean in terms of those who are at high risk? There are a lot of people in South Africa who are neither vaccinated nor previously had infection. We just haven’t seen, even with this dynamic transmission, that population coming to medical care and needing intensive care. Maybe that will change. But given how dynamic the transmission for this virus is — it has to be throughout much of the Johannesburg-Pretoria area — you would think immune-compromised individuals with HIV who have not yet been infected or vaccinated would be presenting for medical care.
And I’m looking at all of these other groups. Look at the outbreaks in Oslo, Denmark, or the U.K. Granted, a number of those situations were in highly vaccinated populations. We surely have data supporting that there were a lot of breakthroughs, no question about it, a remarkable number of breakthroughs in people who were fully vaccinated. What we don’t know yet is how many had boosters. The point is, even with that, there was still a lack of severe cases. I think that’s great news. Now the question is how will that extrapolate into those who are immune compromised, those who are not vaccinated, those who have underlying comorbidities. I think that’s what we’re still waiting to find out.
Should we change the definition of fully vaccinated to include only those people who have received three shots?
I’ve been saying that since August! You may recall last March and April, I was not very popular when I promoted heavily the idea of one dose now and a wait of ten-to-12 weeks for dose two because of the data from the U.K. looking at Alpha. It was very clean and clear at that point with Alpha that we were seeing a reduction in serious illness in the U.K. with one dose. People kept saying, “No, no, no, you have to keep the three-to-four-week second-dose regimen.” It never made sense to me because if you look at vaccine immunology, it would suggest that spacing the doses out would give you a much better immune response. Sure enough, the data have shown that in the U.K. and Canada, where they did wait ten-to-12 weeks.
Eric Topol and I did a piece in the Washington Post on this very issue. I think the data are clear and compelling. All along, I’ve said it should be a three-dose prime and a two-dose prime for the mRNA and adenovirus platforms both. There’s no debate anymore. Everyone recognizes that, with Omicron, we clearly need to have that third dose on the board. This was not a luxury dose, unlike what was described by the WHO and others. It never was.
How long will it take for Omicron to overtake Delta?
I think Omicron is going to be remarkable in how fast it takes. If you look at what it took for Alpha and Delta to prevail, it took really two months before they became the dominant variants around the world, some countries sooner than others. I think you’re going to see this one become the dominant variant in just a matter of weeks.
So as soon as we understand the severity of illness and immune escape, we’ll know what the next year is going to look like.
Absolutely. On the optimistic side, wouldn’t it be an amazing turn of events if Mother Nature herself helps us out by giving us a virus that is much more transmissible, that will win the virus King of the Hill debate, and at the same time give us milder illness? We don’t know that, but it’s surely a possibility. On the other hand, we can still be in deep trouble even if we have less severe illness, just based on the increased transmissibility. Transmissibility offsets severity, so you could have just as many ICUs overrun if, in fact, it’s a less severe illness. We’re still trying to understand breakthroughs, not only for healthy individuals but for the immune compromised or those who have underlying health challenges that put them at increased risk. We don’t know, at this point, how they’re going to fare with this variant.
More on omicron
- What to Know About the New COVID Booster Shots
- The Dismantling of Hong Kong
- What We Know About All the Omicron Subvariants, Including BA.2.12.1